
Hybrid ablation of atrial fibrillation improves patient quality of life: results from the AFEQT questionnaire
Highlight box
Key findings
• A totally thoracoscopic hybrid ablation (HA) approach is associated with a significant 12-month improvement in patient quality of life (QOL) as measured by the Atrial Fibrillation Effect on QualiTy-of-life (AFEQT) questionnaire.
• Rhythm success with HA [<30 seconds atrial fibrillation/flutter/tachycardia (AF/AFl/AT) with or without anti-arrhythmia drug]: 93%.
What is known and what is new?
• A hybrid approach is associated with improved rhythm outcomes compared to isolated endocardial catheter ablation.
• Limited data exist regarding the impact of a HA on patient QOL with AF specific elements.
What is the implication, and what should change now?
• Successful restoration of normal sinus rhythm may not only prevent future stroke, heart failure and dementia but also improve patient QOL.
• Future assessments of surgical ablation effectiveness should incorporate both rhythm success and AF related QOL.
Introduction
Background
Atrial fibrillation (AF) is the most common cardiac arrythmia and affects nearly 3 million people in the United States and is expected to double by 2050 (1). Effective treatment strategies not only restore normal sinus rhythm (2), reduce AF burden (3), mitigate stroke risk (4), improve heart failure (5), decrease the risk of dementia (6), and increase long-term survival (7) but importantly, also improve patient quality of life (QOL) (8). The Atrial Fibrillation Effect on QualiTy-of-life (AFEQT) questionnaire is a validated self-administered health-related questionnaire design to assess the impact of AF on a patient’s QOL (9). A hybrid ablation (HA) strategy uses a 2-stage approach by a team of arrythmia surgeons and an electrophysiologists to target epicardial and endocardial ablation sites via minimally invasive thoracoscopy and catheter ablation. Several recent randomized control studies (10-12) have demonstrated the electrophysiologic advantage of treating complex AF patients with a HA over an isolated endocardial catheter ablation however, there is a paucity of data examining the impact of a HA on patient QOL using the AFEQT questionnaire.
Rationale and knowledge gap
The totally thoracoscopic HA approach is a combination of epicardial and endocardial lesions that nearly replicates the traditional “Cut-N-Sew” Cox-Maze surgical elements (13). Key lesions often omitted from this hybrid approach include the intracaval ablation connecting the superior vena cava and the inferior vena cava; the right atrial appendage lesion; the right atrial free wall or “T” lesion; and the tricuspid isthmus lesion at the “2 o’clock” position. The ability to achieve an effective lesion set with the use of video-assisted thoracoscopic surgery (VATS) techniques and without the use of cardio-pulmonary bypass makes it an attractive option for both referring physicians and patients alike. However, there are limited studies examining the QOL impact of a HA approach. The AFEQT questionnaire is a specific validated survey that evaluates changes in symptoms, daily activities, treatment concerns and treatment satisfaction for patients undergoing treatment for AF.
Objective
We have previously demonstrated the safety and efficacy of our HA approach on the treatment of AF (13). In this study, we seek to determine whether, in the hands of an experienced hybrid team, the HA approach also provides an improvement in patient QOL using the validated AF questionnaire (AFEQT). We present this article in accordance with the STROBE reporting checklist (available at https://vats.amegroups.com/article/view/10.21037/vats-23-64/rc).
Methods
Study population
All adult (age ≥18 years) HA patients who completed both the pre- and 12-month post AFEQT questionnaires from 2017–2019 were included in this study. A total of 74 matched pre- and 12-month post AFEQT questionnaires were analyzed.
Data collection
Patient demographics and standard-post-surgical outcomes were collected via an Adventist Health independent 3rd party data abstraction team and inserted into our Society of Thoracic Surgeons (STS) database. AF specific outcomes [i.e., anti-arrhythmia drugs (AADs) use, anti-coagulation use, etc.] were collected via our data team (co-authors: M.D., S.B., A.P.) and inserted into our password protected secure institutional AF database. The AFEQT questionnaire was prospectively administered pre- and 12-month post-operatively to our HA treated patients over a 3-year period (2017–2019). The results of the AFEQT questionnaire, STS database and AF database were then combined to provide complete patient data for the purposes of this study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Adventist Health-Saint Helena Institutional Review Board approved this study on 1/21/2020 and individual consent for this retrospective analysis was waived.
AFEQT questionnaire
The AFEQT questionnaire includes 20 questions, each answered on a Likert scale from 1 to 7. Calculated AFEQT scores exist from 0–100, with “0” representing maximum disability and “100” representing no disability. Four subscale types exist with the AFEQT assessment: patient symptoms (questions 1–4), daily activities (questions 5–12), treatment concerns (questions 13–18) and treatment satisfaction (questions 19–20).
Rhythm monitoring
Rhythm monitoring was performed by the Saint Helena Hospital Arrhythmia Center team at regular intervals of 3- and 12-month post-operatively (after a 3-month blanking period) and annually thereafter and monitored by the AF nurse navigator. Rhythm data were obtained from standard permanent pacemaker (PPM) interrogations and transdermal Ziopatch monitors, which provide continuous 24-h rhythm data for up to 14-day. Rhythm data were then reviewed by our research team and adjudicated as a “rhythm success” if it met Heart Rhythm Society (HRS) criteria of less than 30 seconds of AF/atrial flutter/atrial tachycardia (AF/AFl/AT) without the use of class I or III AAD.
iRhythm Zio patch monitoring is an industry standard transdermal electrogram monitoring device that provides 24-h of continuous electrogram monitoring for up to 14-day. iRhythm provides patient rhythm monitor reports at the end of patch use to the prescribing physicians (co-authors: Armin Kiankhooy, S.E., G.H.D.). Pacemaker interrogations were standard practice protocols to evaluate the arrhythmia burden capture by patient PPMs. Rhythm data are inserted into the electronic medical record and adjudicated by the Saint Helena Arrhythmia Team.
HA
HA was performed by our group as previously reported (13). Briefly, a two-stage approach was performed, whereby the first stage included a bilateral VATS off-pump surgical ablation and occlusion of the left atrial appendage. Epicardial ablation included bilateral pulmonary vein isolation, left atrial posterior wall isolation, ligament of Marshall division and mitral isthmus ablation. The left atrial appendage was surgically occluded with an AtriClip in all cases. A second stage endocardial catheter ablation was performed 6 weeks after the 1st stage and included confirmation of bilateral pulmonary vein isolation, posterior wall isolation and mitral isthmus ablation as well isolation of the cavo-tricuspid isthmus.
Statical analysis
Statistical analysis was performed using Prism 9.2.0 (GraphPad Software, San Diego, CA, USA). Variables are reported as mean with standard deviation unless otherwise noted. Differences in continuous variables were analyzed using the unpaired nonparametric Mann-Whitney comparative ranks test. Differences in proportions of categorial variables were determined with the Fisher’s Exact test. All P values are two-sided with significance defined as <0.05.
Results
Patient demographics
Complete patient demographics are described in Table 1. Most patients were male 58/74 (78%) and the majority suffered from non-paroxysmal AF (5% paroxysmal, 38% persistent, 57% long-standing persistent). The average time in AF prior to HA was 5.5±5.6 years. The average pre-HA left ventricular ejection fraction (LVEF)% was 50±11 and left atrial size was 4.7±0.8 cm. Most patients at the time of surgery were maintained on oral anticoagulation therapy prior to HA (69/74, 93%) and 45% were on class I or III AAD, the remaining 55% had been transitioned to rate control agents after failing prior class I or III AAD under the supervision of their referring physician. Pre-operative pacemakers were present in 20% of patients.
Table 1
| Variable | Value |
|---|---|
| Age (years) | 68±9.7 |
| BMI (kg/m2) | 32±6.6 |
| Gender (male:female) | 58:16 |
| LVEF% | 50±11 |
| LA size (cm) | 4.7±0.8 |
| AF | |
| Paroxysmal | 4 (5.4) |
| Persistent | 28 (37.8) |
| Long standing persistent | 42 (56.8) |
| Time in AF (years) | 5.5±5.6 |
| Pre-procedural | |
| Oral anticoagulation | 69 (93.2) |
| Class 1 or 3 AAD | 33 (44.6) |
| Pacemaker | 15 (20.3) |
| CHA2DS2-VASc score | 2.7±1.3 |
| HASBLED score | 2.9±1.1 |
Data are presented as mean ± SD or n (%). BMI, body mass index; LVEF, left ventricular ejection fraction; LA, left atrial; AF, atrial fibrillation; AAD, anti-arrhythmia drug.
Procedural outcomes
Procedural outcomes are outlined in detail in Table 2. At the 12-month follow-up, sixty-nine patients (93%) achieved restoration of normal sinus rhythm with <30 seconds of AF/AFl/AT with or without class I or III AAD. Fifty-six (76%) patients achieved restoration of normal sinus rhythm with <30 seconds of AF/AFl/AT without class I or III AAD. Within the 12-month follow-up period two patients underwent repeat endocardial ablation of the mitral isthmus and cavo-tricuspid isthmus lesions. No 30-day deaths or strokes occurred. One temporary phrenic nerve palsy occurred. Three (4%) patients required new permanent pacemakers due to post-ablation sick sinus syndrome.
Table 2
| Variable | Value |
|---|---|
| 12-month rhythm success | |
| NSR success (<30 seconds AF/AFl/AT, on/off AAD) | 69 (93.2) |
| HRS success (<30 seconds AF/AFl/AT, off AAD) | 56 (75.7) |
| Procedural data | |
| VATS operative time (minutes) | 98±25 |
| Post-VATS length of stay (days) | 3.1±1.3 |
| Discharged in NSR post-VATS | 68 (91.9) |
| Catheter ablation time (minutes) | 95±44 |
| New PPM | 3 (4.1) |
| 30-day post HA death or stroke | 0 (0) |
Data are presented as mean ± SD or n (%). NSR, normal sinus rhythm; AF/AFl/AT, atrial fibrillation/atrial flutter/atrial tachycardia; AAD, anti-arrhythmic drug; HRS, Heart Rhythm Society; VATS, video-assisted thoracoscopic surgery; PPM, permanent pacemaker; HA, hybrid ablation.
AFEQT questionnaire
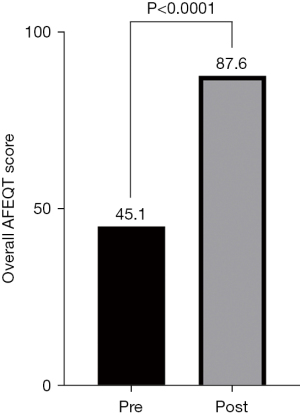
The overall AFEQT score improved significantly from pre- to 12-months post HA [45.1 vs. 87.6, mean of differences 42.5, 95% confidence interval (CI): 36.2–48.8, P<0.0001] (Figure 1). Each subscale AFEQT score also improved significantly from pre- to 12-month post HA (Figure 2). The greatest improvement occurred in the Treatment Concerns Subscale (26.6 vs. 86.0, mean difference 59.5, 95% CI: 52.2–66.7, P<0.0001). This Subscale included questions 13–18; #13 Feeling worried or anxious that your AF can start anytime; #14 Feeling worried that AF may worsen other medical conditions in the long run; #15 Worrying about the treatment side effects from medications; #16 Worrying about complications or side effects from procedures like catheter ablation, surgery, or pacemakers therapy; #17 Worrying about side effects of blood thinners such as nosebleeds, bleeding gums when brushing teeth, heavy bleeding from cuts, or bruising; #18 Worrying or feeling anxious that your treatment interferes with your daily activities. Although, not statistically significant, patients who achieved normal sinus rhythm (NSR) experienced a better overall AFEQT score compared to those patients that remained in AF (NSR, n=69 AFEQT Score 88.2 vs. AF, n=5 AFEQT Score 80.2). At the time of the 12-month post survey; 92% of patients were off class I or III AAD and 81% were off oral anticoagulation medications.

Discussion
Key findings
Patients who underwent a HA approach experienced significant improvements across all domains of the AF specific QOL AFEQT questionnaire. The greatest improvement occurred within the subscale addressing patient “Treatment Concerns”.
Strengths and limitations
The current study provides a contemporary evaluation of the results of a non-sternotomy, non-thoracotomy hybrid team approach to the treatment of AF. The totally thoracoscopic HA approach is less invasive than a standard midline sternotomy or thoracotomy approach for surgical ablation and obviates the need for cardiopulmonary bypass. By eliminating the significant incisional healing, rehabilitation and other adverse effects associated with a sternotomy or thoracotomy, this study is uniquely positioned to not only evaluate the standard rhythm success of AF treatment but also evaluate patient QOL more acutely (12-month) without delay or the impact of sternotomy or thoracotomy-related QOL related-factors. The higher success rate of a HA approach also allows for a direct understanding of the QOL impact of restoring normal sinus rhythm, as only a minority of patients (7%) in our study did not achieve normal sinus rhythm. The main limitation of our study is the small study cohort of seventy-four total patients. Given that the majority of achieved normal sinus rhythm (93%), we were not powered sufficiently to provide a clinically useful comparison of QOL outcomes between patients achieving normal sinus rhythm versus those remaining in AF. The AFEQT questionnaire is also a self-administered survey and is vulnerable to patient perceived treatment bias.
Comparison with similar researches
Only a single prior study from Osmancik et al. (14) from the Czech Republic has examined the totally thoracoscopic HA approach in terms of rhythm success and QOL with the AFEQT questionnaire. In their 75-patient cohort, they similarly reported significant increases in the overall and subscale AFEQT scores of patients who achieved normal sinus rhythm or paroxysmal AF. They did not observe an improvement in AFEQT scores in patients who remained in “permanent” AF.
Although no additional HA studies have evaluated QOL with the AFEQT questionnaire, prior catheter ablation studies have also observed significant improvements in AFEQT score related to decreases AF burden. More impactful changes in QOL in patients who experiences less AF (15,16). Unfortunately, we found no studies examining QOL with the AFEQT questionnaire following open surgical ablation (Cox-Maze).
Explanation of findings
Overall AFEQT and Subscale Scores significantly improved for patients who underwent a HA approach for the treatment of AF. The Subscale category of “Treatment Concerns” was most impacted. This specific subscale finding suggests that beyond just restoration of normal sinus rhythm, patients are most concerned with medication related adverse effects and possible complications. In our experience, these concerns are often centered around two major concerns—end organ dysfunction from class I or III AAD (i.e., thyroiditis, liver fibrosis, pulmonary fibrosis, sick sinus syndrome) or complications from oral anticoagulation medications (i.e., superficial epidermal bleeding and visceral bleeding—gastrointestinal or cerebral) despite the embolic stroke protection that these agents offer. Class I or III AAD usage was significantly reduced in the HA approach, with only 8% of patients reporting AAD use at the time of the 12-month post AFEQT questionnaire. Similarly, all patients received management of the left atrial appendage with an epicardial occlusion device at the time of the HA approach, and consequently 81% were off oral anticoagulation medications at the time of the post 12-month survey. These two main medication category changes in the setting of the HA approach, may be the greatest determinants in the AF patients QOL.
Implications and actions needed
Beyond freedom from AF and its minimally invasive approach, patients treated with the HA strategy appear to gain the most QOL benefit from the ability to reduce class I or III AAD and the need for oral anticoagulation medications with successful management of the left atrial appendage. Our findings highlight the importance of continually and systematically evaluating physiologic responses to treatments rendered and their effects on patient QOL. Future studies evaluating response to AF treatments should include validated AF centered QOL evaluations (i.e., AFEQT) in addition to standard rhythm monitoring.
Conclusions
A totally thoracoscopic HA team approach for the treatment of AF provides a unique opportunity for patients to experience significantly improved QOL with a high rate of sinus rhythm restoration.
Acknowledgments
Funding: This work was supported by an institutional (Adventist Health – Saint Helena) research grant from AtriCure® (Mason, Ohio; USA) which provided salary support hospital employed research assistants (S.B., M.D., A.P.).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://vats.amegroups.com/article/view/10.21037/vats-23-64/rc
Data Sharing Statement: Available at https://vats.amegroups.com/article/view/10.21037/vats-23-64/dss
Peer Review File: Available at https://vats.amegroups.com/article/view/10.21037/vats-23-64/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://vats.amegroups.com/article/view/10.21037/vats-23-64/coif). Armin Kiankhooy serves as an unpaid editorial board member of Video-Assisted Thoracic Surgery from April 2023 to March 2025. All authors report that this work was supported by an institutional (Adventist Health-Saint Helena) research grant from AtriCure® (Mason, OH, USA) and provided salary support hospital employed research assistants (S.B., M.D., A.P.). Armin Kiankhooy has COI with AtriCure and provides consultation services; receives honoraria, travel and meeting support; and participates with the Advisory Board. S.E. has COI with AtriCure and provides consultation services and receives honoraria. G.H.D. has COI with AtriCure and provides consultation services; receives honoraria, travel and meeting support. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Adventist Health – Saint Helena Institutional Review Board approved this study on 1/21/2020, and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370-5. [Crossref] [PubMed]
- Badhwar V, Rankin JS, Damiano RJ Jr, et al. The Society of Thoracic Surgeons 2017 Clinical Practice Guidelines for the Surgical Treatment of Atrial Fibrillation. Ann Thorac Surg 2017;103:329-41. [Crossref] [PubMed]
- Marrouche NF, Brachmann J, Andresen D, et al. Catheter Ablation for Atrial Fibrillation with Heart Failure. N Engl J Med 2018;378:417-27. [Crossref] [PubMed]
- Whitlock RP, Belley-Cote EP, Paparella D, et al. Left Atrial Appendage Occlusion during Cardiac Surgery to Prevent Stroke. N Engl J Med 2021;384:2081-91. [Crossref] [PubMed]
- Kiankhooy A, Pierce C, Burk S, et al. Hybrid ablation of persistent and long-standing persistent atrial fibrillation with depressed ejection fraction: A single-center observational study. JTCVS Open 2022;12:137-46. [Crossref] [PubMed]
- Bunch TJ. Atrial Fibrillation and Dementia. Circulation 2020;142:618-20. [Crossref] [PubMed]
- Iribarne A, DiScipio AW, McCullough JN, et al. Surgical Atrial Fibrillation Ablation Improves Long-Term Survival: A Multicenter Analysis. Ann Thorac Surg 2019;107:135-42. [Crossref] [PubMed]
- Maesen B, van der Heijden CAJ, Bidar E, et al. Patient-reported quality of life after stand-alone and concomitant arrhythmia surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg 2022;34:339-48. [Crossref] [PubMed]
- Spertus J, Dorian P, Bubien R, et al. Development and validation of the Atrial Fibrillation Effect on QualiTy-of-Life (AFEQT) Questionnaire in patients with atrial fibrillation. Circ Arrhythm Electrophysiol 2011;4:15-25. [Crossref] [PubMed]
- DeLurgio DB, Crossen KJ, Gill J, et al. Hybrid Convergent Procedure for the Treatment of Persistent and Long-Standing Persistent Atrial Fibrillation: Results of CONVERGE Clinical Trial. Circ Arrhythm Electrophysiol 2020;13:e009288. [Crossref] [PubMed]
- van der Heijden CAJ, Weberndörfer V, Vroomen M, et al. Hybrid Ablation Versus Repeated Catheter Ablation in Persistent Atrial Fibrillation: A Randomized Controlled Trial. JACC Clin Electrophysiol 2023;9:1013-23. [Crossref] [PubMed]
- Doll N, Weimar T, Kosior DA, et al. Efficacy and safety of hybrid epicardial and endocardial ablation versus endocardial ablation in patients with persistent and longstanding persistent atrial fibrillation: a randomised, controlled trial. eClinicalMedicine 2023;61:102052. [Crossref] [PubMed]
- Dunnington GH, Pierce CL, Eisenberg S, et al. A heart-team hybrid approach for atrial fibrillation: a single-centre long-term clinical outcome cohort study. Eur J Cardiothorac Surg 2021;60:1343-50. [Crossref] [PubMed]
- Osmancik P, Budera P, Talavera D, et al. Improvement in the quality of life of patients with persistent or long-standing persistent atrial fibrillation after hybrid ablation. J Interv Card Electrophysiol 2020;57:435-42. [Crossref] [PubMed]
- Samuel M, Khairy P, Champagne J, et al. Association of Atrial Fibrillation Burden With Health-Related Quality of Life After Atrial Fibrillation Ablation: Substudy of the Cryoballoon vs Contact-Force Atrial Fibrillation Ablation (CIRCA-DOSE) Randomized Clinical Trial. JAMA Cardiol 2021;6:1324-8. [Crossref] [PubMed]
- Gupta D, Vijgen J, Potter T, et al. Quality of life and healthcare utilisation improvements after atrial fibrillation ablation. Heart 2021;107:1296-302. [Crossref] [PubMed]
Cite this article as: Kiankhooy A, Kiankhooy A, Own A, Sertic F, Daw M, Eisenberg S, Burk S, Phillips A, Dunnington GH. Hybrid ablation of atrial fibrillation improves patient quality of life: results from the AFEQT questionnaire. Video-assist Thorac Surg 2024;9:2.


