
Pulmonary resection using polyglycolic acid sheet without fibrin glue and its surgical complications
Highlight box
Key findings
• Pulmonary resection without fibrin glue could be considered an alternative method.
• Prolonged air leakage (PAL) for >7 days including six cases that required reoperation cases: 5.0%.
What is known and what is new?
• A fibrin glue has been used with polyglycolic acid (PGA) sheets to prevent air leakage and pulmonary fistula after pulmonary resections; however, comparisons of outcomes with or without fibrin glue have not been reported.
• Postoperative complications of pulmonary resection using PGA sheet without fibrin glue: 2.4% (readmissions and re-operations).
What is the implication, and what should change now?
• Pulmonary resections using PGA sheets without fibrin glue could be one of the options for preventing PAL.
Introduction
In 2016, in Japan, 31,365 and 5,136 cases of anatomical pulmonary resections via lobectomies and segmentectomies, respectively, were performed (1). Prolonged air leakage (PAL) is one of the most common complications of pulmonary resections. In the 1990s or 2000s, several randomized studies on synthetic sealants (2-4) and fibrin glue in lung surgery revealed the significance of fibrin glue in terms of postoperative air leakage (4). Recently, fibrin glue has been used with polyglycolic acid (PGA) sheets to prevent air leakage and pulmonary fistulas after pulmonary resections. Visceral pleural repairs using PGA combined with fibrin glue were reported to be tolerable at bursting pressures higher than 40 cmH2O (5). However, the efficacy of PGA sheets or oxidized regenerated cellulose (ORC) mesh was reported without fibrin glue and autologous blood (6). If fibrin glue is not always necessary, a postoperative course without it would be acceptable, and the medical cost and blood donation could be reduced.
At our institution, a PGA sheet is attached to the surface of the lung or staple line with blood, saline, or lavage, and fibrin glue is not used due to infectious concerns, complicated procedures, and medical costs [The redemption price of Neobeil sheet is 167 yen per 1 cm2 (10×5 cm; 8,350 JY). If fibrin glue is used, usually a 3ml kit with 33,459 JY cost is needed].
This study aimed to retrospectively reveal the efficacy of PGA sheets without fibrin glue for pulmonary resections and to compare the hospital period with or without reinforcement. Thus, a comparison between whether using a PGA sheet with fibrin glue or covering a PGA sheet without suturing pleural defects is sufficient. We present this article in accordance with the STROBE reporting checklist (available at https://vats.amegroups.com/article/view/10.21037/vats-23-51/rc).
Methods
This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional review board of Saku Central Hospital (No. R201907-07) and individual consent for this retrospective analysis was waived. We retrospectively reviewed 659 consecutive operations from 2013 to 2018 and the clinical courses after pulmonary resections. The inclusion criteria were operations for lung tumors, and the exclusion criteria were pneumonectomies or partial resections (wedge resections), and operations for infectious lesions. The patients who were complicated with postoperative chylothoraces were also excluded, and a total of 483 patients were enrolled in this study. The clinical data analyzed included age, sex, smoking history, comorbidities [chronic obstructive pulmonary disease (COPD) or interstitial pneumonia], type of operation, histopathological diagnoses, chest drainage duration, and length of hospital stay. For logistic regression analysis, patients were divided into two groups: those whose respiratory function test was graded as Global Initiative for Chronic Obstructive Lung Disease (GOLD) and GOLD 2 or more. Interstitial pneumonia was judged as the usual pneumonia pattern, ground-glass opacity, and honeycomb appearance on computed tomography (CT).
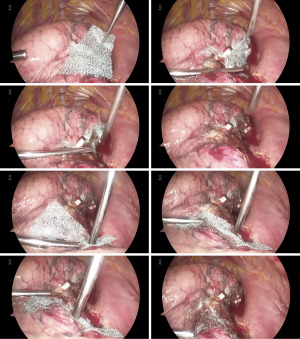
The surgical procedures were as follows: in lobectomy or segmentectomy, auto-suture devices were used for interlobar fissure or segmental formation (resection) and resection of the bronchus and pulmonary artery or vein. After pulmonary resection and lymph node dissection, a sealing test (leak test) was performed at inspiratory pressures of 15–20 cmH2O. If air leakage was observed, mattress sutures with pledget sheets holding the leak point were performed, and the surgeon applied sutures only or covered the pleural injury with a PGA sheet after the 2nd or 3rd sealing tests. If minor air leakage was observed, covering the staple line with a PGA sheet was selected. If no air leakage was observed, the surgeon applied no reinforcements at all. The PGA sheet was 5×10 cm in size, 0.3 mm in thickness (Neoveil sheet® NV-M-3G, Gunze, Osaka, Japan), and was usually cut into four pieces. Each piece was approximately 5×2.5 cm in size. Usually, fibrin glue was not used to fix the PGA sheet; instead, the PGA sheet was fixed with intrathoracic blood or lavage. A cotton stick was not adequate for intertangles because they catch and intertangle with each other; therefore, an opposite stick, an outer cylinder (Endo Finger®, Kenzmedico, Saitama, Japan), was used to catch and release a small amount of saline or blood for adopting the PGA sheet. However, fibrin glue was used during the reoperation, and a fibrin sealant patch (TachoSil® CSL Behring K.K., PA, USA) was used for pulmonary artery bleeding. Another type of PGA sheet (Neoveil Nano®, Gunze) was not used during this period.
For postoperative management, a 20-Fr chest tube (Argyle, Cardinal Health Inc., OH, USA) was placed, and a chest drainage bag (Sumitomo Bakelite Co., Tokyo, Japan) was kept under water pressure as a sealant if the subcutaneous emphysema was tolerable. Otherwise, reinsertion of the chest drainage tube from the anterior and superior intercostal spaces was required. Talc or adhesive materials were not used, and reoperation was performed to close the pulmonary fistula if the patient accepted it after 7–10 days of observation.
Statistical analysis
For comparisons between methods using PGA sheets and drainage or hospital stay, statistical analyses with a t-test or the Kruskal-Wallis test were performed. Associations between PAL for >7 days and clinicopathological variables were analyzed using the chi-squared test for categorical variables. The significance of clinicopathological variables in differentiating risk factors for PAL was assessed using logistic regression analysis. Multivariate logistic regression analysis was performed to identify significant clinicopathological variables (P<0.1) in the univariate analysis. For all analyses, statistical significance was set at P<0.05. JMP software (13.1.0 SAS Institute, Cary, NC, USA) was used for all analyses.
Results
Patient population and procedures
The demographic characteristics and histopathological diagnoses of the 483 patients are shown in Table 1. There were 454 cases of lung cancer (adenocarcinoma, 257; adenocarcinoma in situ, 18; minimally invasive adenocarcinoma, 39; squamous cell carcinoma, 94; adenosquamous, 8; pleomorphic carcinoma, 8; anaplastic carcinoma, 1; pulmonary blastoma, 1; large cell carcinoma and large cell neuroendocrine carcinoma, 12; small cell carcinoma, 11; carcinoid, 5), 27 cases of metastatic tumors (colorectal cancer, 18; other organ cancer, 9), and 2 cases of other lung tumors (B-cell lymphoma, 1; sclerosing hemangioma, 1). Figure 1 shows the technique used to patch the PGA sheet around the pulmonary staple stump.
Table 1
| Variable | No. of patients |
|---|---|
| Age (years), median [range] | 72 [21–88] |
| Sex | |
| Female | 175 |
| Male | 308 |
| Smoking | |
| Never smoker | 160 |
| Smoker | 323 |
| Underlying disease | |
| COPD | 72 |
| UIP (fibrosis) | 23 |
| Surgery | |
| Open bilobectomy | 7 |
| Thoracoscopic lobectomy | 342 |
| Open lobectomy | 38 |
| Thoracoscopic segmentectomy | 91 |
| Thoracoscopic lobectomy + segmentectomy | 5 |
| Pathological diagnosis | |
| Lung cancer | 454 |
| Adenocarcinoma/MIA/AIS | 257/39/18 |
| Squamous cell carcinoma | 94 |
| LCNEC†/small/carcinoid | 12/11/5 |
| Adenosquamous/pleomorphic‡ | 8/10 |
| Metastatic lung tumor | 27 |
| Colorectal cancer | 18 |
| Other organ cancer | 9 |
| Others§ | 2 |
†, LCNEC includes large cell carcinoma; ‡, pleomorphic (n=8), anaplastic (n=1), pulmonary blastoma (n=1); §, B-cell lymphoma (n=1), and sclerosing hemangioma (n=1). COPD, chronic obstructive pulmonary disease; UIP, usual interstitial pneumonia; MIA, minimally invasive adenocarcinoma; AIS, adenocarcinoma in situ; LCNEC, large cell neuroendocrine carcinoma.
Postoperative results
Of the 483 major lung resections, thoracoscopic lobectomy was performed in 342 cases, thoracoscopic segmentectomy in 91, thoracoscopic lobectomy + segmentectomy in 5, open lobectomy in 38, and bilobectomy in 7. Total complications associated with air leakage, including readmission caused by subcutaneous emphysema, were seen in 29 cases (6.0%).
Complications details and rates
There were 5 readmissions for subcutaneous emphysema (1.0%) and 7 re-operations (1.4%) for one case with a broncho-pleural fistula and six cases of pulmonary fistulas. The average postoperative drainage duration was 2.9 (median 2) days, and the average postoperative hospital stay was 7.3 (median 6) days. PAL for >7 days was observed in 24 cases (5.0%), including six cases that required reoperation. The postoperative drainage period for patients in whom the PGA sheet was used was longer than that for patients in whom reinforcement was not needed (3.00 days for PGA sheet vs. 2.49 days for no use, P=0.0429, t-test; 3.13 days for suture + PGA sheet vs. 2.49 days for no use, P=0.0034), although there was no difference between that for patients whom the PGA sheet was used and that for patients in whom the PGA sheet was not used (3.00 days for PGA sheet vs. 2.98 days for suture only, P=0.9535, t-test; 3.13 days for suture + PGA sheet vs. 2.98 day for suture only, P=0.0034). The number of PALs was significantly lower (2–8% vs. 1–5%) in groups without a PGA sheet (Table 2).
Table 2
| Variable | None (n=103) | Suture only (n=58) | Suture + PGAS (n=217) | PGAS (n=105) | P value |
|---|---|---|---|---|---|
| Drainage duration (days) | 2.5±0.9 | 3.0±1.6 | 3.1±1.9 | 3.0±2.3 | 0.0249 |
| Air leakage of >7 days | 1 (1.0) | 3 (5.2) | 18 (8.3) | 2 (1.9) | 0.0137 |
| Hospital days | 6.3±2.9 | 8.6±12.0 | 8.6±12.0 | 6.8±4.6 | 0.3090 |
Data are presented as No. (%) or mean ± standard deviation. P values were calculated using the Kruskal-Wallis test. PGAS, PGA sheet patching without fibrin glue.
Regression analysis on complications of PAL
Univariate logistic regression analysis showed that PAL of >7 days was more often observed in male patients [odds ratio (OR) =14.04, 95% confidence interval (CI): 2.92–252.2, P=0.0001], smokers (OR =5.774, 95% CI: 1.67–36.3, P=0.0032), or patient with interstitial pneumonia (OR =4.632, 95% CI: 1.26–13.8, P=0.0241). The multiple logistic regression analysis did not include the use of PGA sheets without fibrin glue, but male sex was identified as a significant risk factor (OR =8.95, 95% CI: 1.40–180.2, P=0.0164) and the presence of interstitial pneumonia was a borderline significant risk factor (OR =3.57, 95% CI: 0.94–11.2, P=0.0608) (Table 3).
Table 3
| Variables | n | Univariate LR | Multivariate LR | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |||
| Sex | ||||||
| Female | 175 | 1 | 0.0001 | 1 | 0.0164 | |
| Male | 308 | 14.04 (2.92–252.2) | 8.95 (1.40–180.2) | |||
| Age (years) | ||||||
| ≤71 | 245 | 1 | 0.7292 | |||
| ≥72 | 238 | 1.156 (0.51–2.68) | ||||
| Smoker | ||||||
| Never | 160 | 1 | 0.0032 | 1 | 0.7121 | |
| Smoker | 323 | 5.774 (1.67–36.3) | 1.36 (0.31–10.0) | |||
| COPD | ||||||
| − | 411 | 1 | 0.0666 | 1 | 0.2987 | |
| + | 72 | 2.496 (0.93–6.03) | 1.68 (0.61–4.26) | |||
| IP (fibrosis) | ||||||
| − | 460 | 1 | 0.0241 | 1 | 0.0608 | |
| + | 23 | 4.632 (1.26–13.8) | 3.57 (0.94–11.2) | |||
| Surgery | ||||||
| Segmentectomy | 96 | 1 | 0.3275 | |||
| Lobectomy | 387 | 1.779 (0.60–7.64) | ||||
| Surgical site | ||||||
| Upper lobe | 260 | 1 | 0.4210 | |||
| Middle/lower | 223 | 1.401 (0.61–3.25) | ||||
| PGA sheet | ||||||
| − | 159 | 1 | 0.0659 | 1 | 0.1027 | |
| + | 324 | 2.549 (0.94–8.88) | 2.36 (0.85–8.41) | |||
LR, logistic regression; OR, odds ratio; CI, confidence interval; COPD, chronic obstructive pulmonary disease; IP, interstitial pneumonia; PGA, polyglycolic acid.
Discussion
PAL is the most common complication of pulmonary resection. Dezube et al. reported that 5.4% of 2,384 patients who underwent lobectomies, segmentectomies, or wedge resections had PAL for more than 5 days, 22.5% of them required interventions, and 55% required reoperations (7). Hoeijmakers et al. reported that the incidence of PAL for >5 days was 9.0% in 12,382 patients, and intraoperative preventive measures varied between hospitals; in an online survey in the Netherlands, 17.6% of the surgeons used sealants [TachoSil 64.4%, Tissucol (fibrin glue) 76.3%, Neoveil 20.3%, etc.], while 13.2% never used sealants (8).
Pulmonary resection using fibrin glue has been established in the past 20–30 years (2), and a randomized, blinded study showed a lower incidence of alveolar air leakage and shorter duration of chest tube placement and postoperative length of hospital stay. Fibrin glue consists of fibrinogen and thrombin, and its combination with a PGA sheet is thought to be an indispensable agent for pulmonary resection. There have been some reports that compared using PGA sheets with fibrin glue or fibrin glue only; however, no reports have been published to compare PGA sheets with fibrin glue or PGA only (9). Sakai et al. reported that a method using PGA and fibrin glue showed higher bursting pressures than a method using ORC mesh and fibrin glue, ORC mesh only, or fibrin glue alone (5). However, a general concern with fibrin glue is the transmission of blood-borne diseases. Kawamura et al. reported a 20% transmission rate of human parvovirus B19 as a potential pathogen in immunocompromised hosts (10).
Kawai et al. reported a better method of combining PGA sheets with fibrin glue, with a postoperative drainage period of 3.1–4.67 days, and the frequency of air leaks for >7 days was 13.5% (17/126) (11). Kawashima et al. reported the feasibility of autologous fibrin glue with a postoperative drainage period of 3.17–3.23 days, and PAL was observed in 12.8–16.7% of cases (12). In the National Clinical Database in Japan, postoperative PAL of >7 days has been reported in 4.5–5.3% of cases (13). In the present cases, the frequency of PAL for >7 days was 5.0% (24/483), which may be different considering whether the pleural defect was sutured or not. We usually suture pleural defects in which an air leak is observed and possibly thread the edge of the pleura to the opposite pleura to shut the air leak point with a pledget sheet. This might be useful to seal air leaks, although it affects postoperative pulmonary function to a lesser extent than that of the PGA patch to the pleural defect with fibrin glue. However, air leakage was not observed at inflation pressures >20 cmH2O, and postoperative air leakage was sometimes observed after extubation. When postoperative air leakage occurs, a PGA sheet may be useful to patch or accelerate adhesion. In some cases of reoperation for PAL, the PGA sheet was not shifted or removed but attached to the pulmonary parenchyma, and the air leak was conducted just under the PGA sheet.
Recently, a linear staple device with bioabsorbable PGA was used for pulmonary wedge resection with emphysema, and postoperative air leakage following pulmonary lobectomy was significantly less frequent in the stapler with PGA group than in the stapler-only group (14).
In surgery for primary spontaneous pneumothoraces, a PGA patch after bullectomy was associated with lower rates of postoperative recurrence and PAL than the non-PGA approach in 1,095 patients, as reported in a systemic review (15). Ozawa et al. reported that the recurrence rate of covering PGA sheets after bullectomy was less than that of covering ORC mesh (post-drainage period, 2.4±1.0 days). In these cases, no fibrin glue was used after lung resections, such as bullectomies (6). Fibrin glue is not necessarily required to fix the PGA sheet and prevent pulmonary fistulas. Pulmonary resection without fibrin glue could be considered an alternative method, although there might be some points to note: (I) the interlobular fissure should be separated to a depth that does not damage the pleura of the remaining pulmonary lobe; (II) a stapler device of appropriate height should be selected; (III) the interlobular fissure should be divided on the remaining pulmonary lobe’s side to avoid leaving a defect.
This study had some limitations. This study is not a prospective comparative analysis between the use of the fibrin glue group and the without fibrin glue group. This study had a retrospective design, was conducted at a single institute, and had a small sample size. In this study, a comparison between using a PGA sheet with fibrin glue or covering a PGA sheet without suturing pleural defects was not sufficient, as cases that required a suture were present in patients with an important intraoperatively identified air leak (Table 2). In severe emphysema cases, rupture of the residual lung is sometimes observed even with a lower pressure inflation test, and these cases should be treated with PGA sheet with fibrin glue to avoid postoperative severe subcutaneous emphysema.
Conclusions
We would not contradict the use of fibrin glue; however, this study concluded that pulmonary resections using PGA sheets without fibrin glue might be tolerable in terms of the postoperative drainage duration and hospital stay.
Acknowledgments
We would like to thank Editage (www.editage.com) for the English language editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://vats.amegroups.com/article/view/10.21037/vats-23-51/rc
Data Sharing Statement: Available at https://vats.amegroups.com/article/view/10.21037/vats-23-51/dss
Peer Review File: Available at https://vats.amegroups.com/article/view/10.21037/vats-23-51/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://vats.amegroups.com/article/view/10.21037/vats-23-51/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional review board of Saku Central Hospital (No. R201907-07) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Committee for Scientific Affairs, The Japanese Association for Thoracic Surgery. Thoracic and cardiovascular surgeries in Japan during 2018: Annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 2021;69:179-212. [Crossref] [PubMed]
- Fleisher AG, Evans KG, Nelems B, et al. Effect of routine fibrin glue use on the duration of air leaks after lobectomy. Ann Thorac Surg 1990;49:133-4. [Crossref] [PubMed]
- Wong K, Goldstraw P. Effect of fibrin glue in the reduction of postthoracotomy alveolar air leak. Ann Thorac Surg 1997;64:979-81. [Crossref] [PubMed]
- Fabian T, Federico JA, Ponn RB. Fibrin glue in pulmonary resection: a prospective, randomized, blinded study. Ann Thorac Surg 2003;75:1587-92. [Crossref] [PubMed]
- Sakai T, Matsutani N, Kanai E, et al. Efficacy of a sheet combined with fibrin glue in repair of pleural defect at the early phase after lung surgery in a canine model. Gen Thorac Cardiovasc Surg 2018;66:103-7. [Crossref] [PubMed]
- Ozawa Y, Sakai M, Ichimura H. Covering the staple line with polyglycolic acid sheet versus oxidized regenerated cellulose mesh after thoracoscopic bullectomy for primary spontaneous pneumothorax. Gen Thorac Cardiovasc Surg 2018;66:419-24. [Crossref] [PubMed]
- Dezube AR, Dolan DP, Mazzola E, et al. Risk factors for prolonged air leak and need for intervention following lung resection. Interact Cardiovasc Thorac Surg 2022;34:212-8. [Crossref] [PubMed]
- Hoeijmakers F, Hartemink KJ, Verhagen AF, et al. Variation in incidence, prevention and treatment of persistent air leak after lung cancer surgery. Eur J Cardiothorac Surg 2021;61:110-7. [Crossref] [PubMed]
- Aprile V, Bacchin D, Calabrò F, et al. Intraoperative prevention and conservative management of postoperative prolonged air leak after lung resection: a systematic review. J Thorac Dis 2023;15:878-92. [Crossref] [PubMed]
- Kawamura M, Sawafuji M, Watanabe M, et al. Frequency of transmission of human parvovirus B19 infection by fibrin sealant used during thoracic surgery. Ann Thorac Surg 2002;73:1098-100. [Crossref] [PubMed]
- Kawai H, Harada K, Ohta H, et al. Prevention of alveolar air leakage after video-assisted thoracic surgery: comparison of the efficacy of methods involving the use of fibrin glue. Thorac Cardiovasc Surg 2012;60:351-5. [Crossref] [PubMed]
- Kawashima M, Kohno T, Fujimori S, et al. Feasibility of autologous fibrin glue in general thoracic surgery. J Thorac Dis 2020;12:484-92. [Crossref] [PubMed]
- Shintani Y, Yamamoto H, Sato Y, et al. A risk model for prolonged air leak after lobectomy using the National Clinical Database in Japan. Surg Today 2022;52:69-74. [Crossref] [PubMed]
- Deguchi H, Tomoyasu M, Shigeeda W, et al. Reduction of air leakage using linear staple device with bioabsorbable polyglycolic acid felt for pulmonary lobectomy. Gen Thorac Cardiovasc Surg 2020;68:266-72. [Crossref] [PubMed]
- Mao Y, Zhang Z, Zeng W, et al. A clinical study of efficacy of polyglycolic acid patch in surgery for pneumothorax: a systemic review and meta-analysis. J Cardiothorac Surg 2020;15:117. [Crossref] [PubMed]
Cite this article as: Endoh H, Yamamoto R, Nishizawa N, Satoh Y. Pulmonary resection using polyglycolic acid sheet without fibrin glue and its surgical complications. Video-assist Thorac Surg 2024;9:4.


