
Diaphragm plication in the era of minimally invasive surgery
Diaphragm paralysis is defined as a loss of muscle tone and elastic properties of the muscle fibers without disruption of diaphragm integrity and/or chest wall attachment. With disease progression, diaphragm paralysis leads to muscular atrophy and fibroelastic tissue deposition resulting in permanent elevation of the dome. Abnormal or delayed fetal myotome migration leads to congenital defect called diaphragm eventration. On the contrary, acquired diaphragm paralysis is a rare entity in adult patients with an incidence of <0.05% and male predominance (1). Although current literature states that acquired paralysis and congenital eventration are different entities and should not be confused, nowadays, terms “eventration”, “relaxation” and “paralysis” are used at times interchangeably. The most effective and radical treatment for symptomatic patients with diaphragmatic paralysis is a diaphragm plication. Conservative management with spontaneous resolution of diaphragm elevation within 6 months after insulting event is effective in no more than 10% of cases (2). However, it may occur in up to 78% of the patients within 2 years after cardiac surgery (3). Thereby, surgical intervention can be delayed in appropriate patients in anticipation of spontaneous recovery. For symptomatic patients, unable to wait for recovery, surgical intervention can be considered earlier. In pediatric population, the main indication for diaphragm plication after cardiac surgery is failure to wean from mechanical ventilation.
In the article “Diaphragmatic plication: current evidence and techniques in the management of the elevated hemidiaphragm”, Gilbert and Wei provided a comprehensive literature review on existing methods of surgical plication, as well as diagnostic methods (4). Over the past decades, different open and minimally invasive approaches for diaphragm plication have been described with significant improvement of oxygenation and spirometry values as well as symptomatic improvement (e.g., decrease in dyspnea on a visual analogue scale) after surgery (5,6). Different plication techniques have been described including interrupted mattress sutures buttressed with Teflon pledgets, U-stitches, stapling, mesh reinforcement with or without diaphragmatic incision for abdominal organs control. Multiple retrospective single-center studies have demonstrated improvement of pulmonary function test values in postoperative period using these techniques at a long-term follow-up (7). The variety of the proposed methods of diaphragm plication determines the need to systematize results of their application in terms of postoperative complications, improvement of functional status and frequency of relapses, as well as implementation and reproducibility of the methods. Despite steadily growing interest in minimally invasive treatment of diaphragm dysfunction, the number of studies that meet rigorous criteria of high level of evidence is not sufficient. As authors correctly mentioned, choice of transthoracic or transabdominal approach remains surgeon-depended.
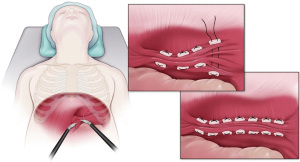
Minimally invasive transthoracic approach is gaining more recognition, especially with availability of robotic technology. In their literature review, authors described in details robotic-assisted transthoracic approach as a preferred technique in their institution using running mattress sutures buttressed with Teflon pledgets (4). Although, benefits of minimally invasive techniques are obvious, some authors mentioned such disadvantages of video-assisted thoracic surgery (VATS) plication as limited workspace due to elevated dome of a paralyzed diaphragm, no difference in postoperative pain compared to open approach, difficulty of obtaining a sufficiently tense diaphragm and an elevated risk of abdominal organs damage (8,9). On the contrary, transabdominal approach allows a better workspace, excellent visual control of the intraabdominal viscera and obviates the need for the lung isolation. In our practice, we prefer robotic transthoracic approach for the right hemidiaphragm plication and transabdominal approach in case of the left-sided procedure (Figure 1) (7,10).
Authors are correct in their conclusion, that currently not a single method could be recommended as a gold standard. Published short- and long-term results of thoracoscopic and laparoscopic approaches are comparable with transthoracic open diaphragm plication outcomes, at the same time offering patients all the advantages of a minimally invasive surgery, potentially with less complications. Hence, preference should be given to minimally invasive approaches, based on individual surgeon’s experience with an procedure and preference.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Video-Assisted Thoracic Surgery. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://vats.amegroups.com/article/view/10.21037/vats-23-49/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Groth SS, Andrade RS. Diaphragmatic eventration. Thorac Surg Clin 2009;19:511-9. [Crossref] [PubMed]
- Mouroux J, Venissac N, Leo F, et al. Surgical treatment of diaphragmatic eventration using video-assisted thoracic surgery: a prospective study. Ann Thorac Surg 2005;79:308-12. [Crossref] [PubMed]
- Summerhill EM, El-Sameed YA, Glidden TJ, et al. Monitoring recovery from diaphragm paralysis with ultrasound. Chest 2008;133:737-43. [Crossref] [PubMed]
- Gilbert A, Wei B. Diaphragmatic plication: current evidence and techniques in the management of the elevated hemidiaphragm. Video-assist Thorac Surg 2023;8:16. [Crossref]
- Graham DR, Kaplan D, Evans CC, et al. Diaphragmatic plication for unilateral diaphragmatic paralysis: a 10-year experience. Ann Thorac Surg 1990;49:248-51; discussion 252. [Crossref] [PubMed]
- Wright CD, Williams JG, Ogilvie CM, et al. Results of diaphragmatic plication for unilateral diaphragmatic paralysis. J Thorac Cardiovasc Surg 1985;90:195-8. [Crossref] [PubMed]
- Gritsiuta AI, Gordon M, Bakhos CT, et al. Minimally Invasive Diaphragm Plication for Acquired Unilateral Diaphragm Paralysis: A Systematic Review. Innovations (Phila) 2022;17:180-90. [Crossref] [PubMed]
- Versteegh MI, Braun J, Voigt PG, et al. Diaphragm plication in adult patients with diaphragm paralysis leads to long-term improvement of pulmonary function and level of dyspnea. Eur J Cardiothorac Surg 2007;32:449-56. [Crossref] [PubMed]
- Celik S, Celik M, Aydemir B, et al. Long-term results of diaphragmatic plication in adults with unilateral diaphragm paralysis. J Cardiothorac Surg 2010;5:111. [Crossref] [PubMed]
- Biswas Roy S, Haworth C, Ipsen T, et al. Transabdominal robot-assisted diaphragmatic plication: a 3.5-year experience. Eur J Cardiothorac Surg 2018;53:247-53. [Crossref] [PubMed]
Cite this article as: Gritsiuta AI, Petrov RV. Diaphragm plication in the era of minimally invasive surgery. Video-assist Thorac Surg 2023;8:24.


