
A case report of massive hemothorax in pregnant woman with a pulmonary arteriovenous malformation: sometimes thoracotomy is the only option?
Highlight box
Key findings
• We report a case of a life-threatening complication due to ruptured of a pAVM in a black pregnant woman treated by surgical approach.
What is known and what is new?
• pAVMs are vascular pathological anomalies due to genetic diseases or associated with underlying pathologic factors. Pregnancy is considered a strong risk factor associated with haemorrhages in patients with arteriovenous fistulas. Embolization is the treatment of choice, but when endovascular management is not feasible, surgical approaches include wedge resection, segmentectomy, lobectomy and pneumonectomy, also performed by video-assisted thoracoscopic surgery (VATS).
• In this report, the rupture of a pAVM resulted in an emergency situation: pregnant patient showed deteriorating haemorrhagic shock with unstable vital signs. Therefore, we decided to perform an emergency thoracotomy, without an exploratory video-assisted thoracoscopy (VATS) first.
What is the implication, and what should change now?
• The difficulties in choosing a treatment strategy, which must be balanced against potential risks to the mother and fetus, need a multidisciplinary approach to the treatment of this condition.
Introduction
Background
Pulmonary arteriovenous malformations (pAVMs) are vascular pathological anomalies due to abnormal communications between pulmonary arteries and veins (1). The main cause of pAVMs is hereditary haemorrhagic telangiectasia (HHT), an autosomal genetic disease that leads to abnormal blood vessel development at multiple sites such as skin, mucous membranes, lungs, liver and brain (2). pAVMs can be also an idiopathic condition, or associated with underlying pathologic factors such as trauma, mitral stenosis, hepatic cirrhosis, metastatic carcinoma, systemic amyloidosis and infections as actinomycosis and schistosomiasis. pAVMs are generally characterized by single or multiple lesions, and they are epidemiologically more frequent in females than in males (3). pAVMs are rare clinical entities and their incidence in the general population is estimated at about 2–3 cases per 100,000. This kind of vascular anomalies are due to genetic conditions (as HHT or Rendu-Osler-Weber syndrome) or associated with other pathological conditions as trauma, hepatic cirrhosis, schistosomiasis, mitral stenosis, previous cardiac surgery, actinomycosis, Fanconi syndrome (Table 1). pAVM could present as single or multiple lesions, unilateral or bilateral (3,4). Chest computed tomography (CT) is an efficient method for the initial diagnosis, because it can show size, number, nature, location and anatomy of pAVM. Most pAVMs are asymptomatic, but they can occasionally cause haemoptysis, dyspnoea, chest pain, hypoxemia and cyanosis, as far as massive haemorrhagic complications. The rupture of a pAVM can be a rare cause of haemothorax with fatal outcomes. Pregnancy is considered a strong risk factor associated with haemorrhages in patients with arteriovenous fistulas, because of increased cardiac output and blood volume, and hormonal changes (1,3). Computed tomography angiography (CTA) is considered the gold standard method for diagnosis and is useful to guide therapeutic choices. It is also necessary in order to define size, number, nature, location and anatomy. Endovascular embolization is the first-line treatment and surgery is sometimes necessary (5).
Table 1
| Congenital causes |
| HHT |
| Idiopathic |
| Acquired causes |
| Trauma |
| Cirrhosis |
| Mitral stenosis |
| Previous cardiac surgery |
| Malignancy |
| Amyloidosis |
| Schistosomiasis/actinomycosis |
| Idiopathic |
pAVM, pulmonary arteriovenous malformation; HHT, hereditary haemorrhagic telangiectasia.
Rationale and knowledge gap
However, in literature, only few reports describe the treatment of pAVMs rupture.
Objective
We report a case of a life-threatening complication due to a ruptured pAVM in a black pregnant woman. We present this case in accordance with the CARE reporting checklist (available at https://vats.amegroups.com/article/view/10.21037/vats-22-44/rc).
Case presentation
We present the case of a 31-year-old black female 24 weeks pregnant who was admitted to the emergency room with sudden chest pain and dyspnoea. There was no history of trauma. Her past medical history included epistaxis episodes and recurrent pregnancy loss. She had no past medical history of HHT.
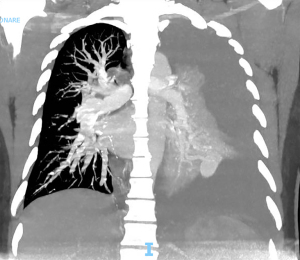
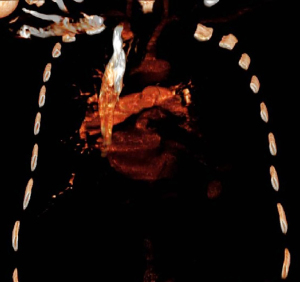
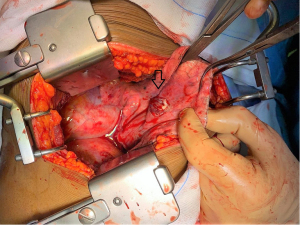
On admission, the patient’s heart rate was 150 beats per minute, blood pressure was 70/50 mmHg, and oxygen saturation was 85% on room air. Blood tests revealed low haemoglobin count (6 g/dL) and thrombocytopenia (100,000 platelets per microliter). Arterial blood gas showed metabolic acidosis. The patient immediately underwent resuscitation with crystalloid infusion and CTA which showed a massive pleural effusion in the left hemithorax with the presence of a large clot. Furthermore, a hyperdense formation on the left lower lobe of 26 mm in contiguity with a pulmonary vessel was found (Figures 1,2). After multidisciplinary discussion (surgeons, gynaecologists and intensive care doctors), the patient was taken to the operating room. After induction of general anaesthesia via a double lumen tube, she underwent a left thoracotomy, access to the thoracic cavity identifying massive haemothorax with aspiration of about 2 L of blood. During surgery a suspected pAVM of dorsal segment of the left lower lobe was identified (Figure 3), therefore a wedge resection of the pathological finding was performed. No other lesions were identified intraoperatively. Two thoracic chest tubes were then placed and operative time was 75 minutes. After surgery the patient was admitted to intensive care unit for close clinical, hemodynamic monitoring and blood transfusions. After three days, once hemodynamic stabilization was achieved and spontaneous ventilation was restored, she was transferred to the obstetrics and gynaecology department until she was discharged home on postoperative day 8. The pregnancy continued regularly and 5 months later a caesarean section was scheduled. The newborn was healthy without complications. Final histological report confirmed a pAVM of the left lower lobe examined.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
pAVMs are rare clinical entities, the three main treatment options are: conservative medical treatment, endovascular embolization and surgical resection. Embolization is the treatment of choice in elective situations. Embolization is indicated in following cases:
- Progressive growth of the lesions;
- Symptomatic hypoxemia;
- Paradoxical embolism;
- Feeding vessels of 3 mm or larger.
After localization of the malformation by angiography it consists in a selective catheterization and embolization of the feeding artery. In a single session multiple pulmonary malformation can be embolized. Recanalization and peri-interventional paradoxical embolism are the main complications of endovascular management. When endovascular management is not feasible, surgery has to be considered (6). Surgical approaches include wedge resection, segmentectomy, lobectomy and pneumonectomy, also performed by video-assisted thoracoscopic surgery (VATS). VATS pulmonary resection is an excellent therapeutic alternative to embolization especially in case of solitary large arteriovenous malformations (7). Surgery becomes mandatory in case of life-threatening haemorrhagic complications, such as massive haemothorax following the rupture of a pAVM. Because of the increased cardiac output and the effects of progesterone on blood vessels, pAVMs are at high risk of rupture or bleeding during pregnancy, especially in the latter two trimesters, with a considerable fatal risk (7,8).
Strengths and limitations
In this report, the rupture of a pAVM resulted in an emergency situation: pregnant patient showed deteriorating haemorrhagic shock with unstable vital signs. Therefore, we decided to perform an emergency thoracotomy, without an exploratory VATS first. Our patient had no medical or genetic history compatible with a diagnosis of HHT. In our case, patient had a full-term pregnancy by scheduled cesarean delivery, in the absence of pathological consequences for the infant.
Comparison with similar researches
Several cases of life-threatening complications from ruptured pAVM in pregnant women are described in literature. The management of this kind of patient includes, in selected cases, early induction of delivery (9). In case of early diagnosis of pAVM, prophylactic embolization of the vascular malformation is possible to avoid severe complications during pregnancy. After endovascular embolization, surgery resection could be scheduled. In other cases of pAVM rupture reported in literature, early induction of delivery was not necessary and emergency surgery was performed by an initial VATS approach.
Implications and actions needed
The choice of treatment depends on: clinical conditions of the pregnant patient, age of the fetus, morphological features, numbers and location of pAVM, risk of complications (10). Our patient was in haemorrhagic shock due to massive pleural blood loss, consequently the situation did not allow the choice of a less invasive therapy. Embolization was not considered because of the patient’s hemodynamic instability and the surgery treatment was performed after careful evaluation together with the anesthesiologists.
Conclusions
In conclusion, the difficulties in choosing a treatment strategy, which must be balanced against potential risks to the mother and fetus, need a multidisciplinary approach to the treatment of this condition. In case of surgery, clinical conditions of the patient and the age of the fetus should be taken in consideration when selecting the approach. Thoracotomy is an effective approach for a prompt management of bleeding in case of patients with unresponsive haemorrhagic shock, especially in case of pregnancy (8).
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://vats.amegroups.com/article/view/10.21037/vats-22-44/rc
Peer Review File: Available at https://vats.amegroups.com/article/view/10.21037/vats-22-44/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://vats.amegroups.com/article/view/10.21037/vats-22-44/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cartin-Ceba R, Swanson KL, Krowka MJ. Pulmonary arteriovenous malformations. Chest 2013;144:1033-44. [Crossref] [PubMed]
- Shovlin CL. Pulmonary arteriovenous malformations. Am J Respir Crit Care Med 2014;190:1217-28. [Crossref] [PubMed]
- Pick A, Deschamps C, Stanson AW. Pulmonary arteriovenous fistula: presentation, diagnosis, and treatment. World J Surg 1999;23:1118-22. [Crossref] [PubMed]
- Ma X, Jie B, Yu D, et al. Massive haemorrhagic complications of ruptured pulmonary arteriovenous malformations: outcomes from a 12 years' retrospective study. BMC Pulm Med 2021;21:230. [Crossref] [PubMed]
- Shovlin CL, Jackson JE. Pulmonary arteriovenous malformations and other vascular abnormalities. In: Mason RJ, Broaddus VC, Martin T, et al. editors. Murray and Nadel’s textbook of respiratory medicine. 5th edition. Philadelphia, PA: Elsevier-Saunders; 2010:1261-82.
- Di Crescenzo V, Napolitano F, Vatrella A, et al. Pulmonary arterovenous malformation causing hemothorax in a pregnant woman without Osler-Weber-Rendu syndrome. Open Med (Wars) 2015;10:549-54. [Crossref] [PubMed]
- Shiiya H, Suzuki Y, Yamazaki S, et al. Polypoid pulmonary arteriovenous malformation causing hemothorax treated with thoracoscopic wedge resection. Surg Case Rep 2018;4:21. [Crossref] [PubMed]
- Esplin MS, Varner MW. Progression of pulmonary arteriovenous malformation during pregnancy: case report and review of the literature. Obstet Gynecol Surv 1997;52:248-53. [Crossref] [PubMed]
- van den Bulck M, Berenger Ngah C, Ntula H, et al. Haemothorax in a Pregnant Woman Secondary to Rupture of a Pulmonary Arteriovenous Malformation. Eur J Case Rep Intern Med 2022;9:003549. [Crossref] [PubMed]
- Naito J, Nakajima T, Morimoto J, et al. Emergency surgery for hemothorax due to a ruptured pulmonary arteriovenous malformation. Gen Thorac Cardiovasc Surg 2020;68:1528-31. [Crossref] [PubMed]
Cite this article as: Ginestri M, Tamburini N, De Troia A, Bonazza S, Carcoforo P, Cavallesco GN. A case report of massive hemothorax in pregnant woman with a pulmonary arteriovenous malformation: sometimes thoracotomy is the only option? Video-assist Thorac Surg 2023;8:19.


