Challenges for pure uniportal robotic-assisted thoracoscopic surgery
Background
The most cutting-edge and recent innovation in the field of robotic-assisted thoracic surgery is pure uniportal robotic-assisted thoracic surgery, or U-RATS. Robotic cameras, dissecting tools, and staplers are used in conjunction with a single incision made in the intercostal space (ICS). A thoracic surgeon controls the robotic system’s patient cart from a master console; the patient cart is linked to three instrumental arms and a camera arm through electrical cables and robotic fibers (1). A very sensitive sensor, capable of filtering out hand tremors, transmits the user’s actions to the cart’s master handles (6-Hz motion filter) (1). The cart arm gives pitch, yaw, and insertion movements, but the Endo wrist offers internal pitch, internal yaw, and rotation movements (1). During this surgery, the ribs are not separated. U-RATS is more useful than multiport because it allows for more effective control of intraoperative bleeding. When U-RATS fails to stop bleeding, the surgeon can quickly undock the device and convert to either U-VATS or a thoracotomy. Surgeons may opt to convert to U-VATS or thoracotomy depending on their level of experience, preference, and the specifics of each patient. Thoracic surgeons are more comfortable with U-RATS, and patients’ recovery is fast and smooth. U-RATS is very important in lung resection and airway reconstruction, with less infection in comparison to other approaches (2,3). For the thoracic surgeon, the U-RATS approach to the carina offers excellent manoeuvrability, accessibility, and precision during carinal resection and reconstruction. In this article, we discuss the current challenges that the uniportal RATS technique is encountering all around the world in the field of thoracic surgery.
Instrumentation and advantages of U-RATS using da Vinci Xi system
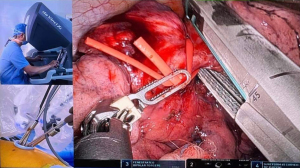
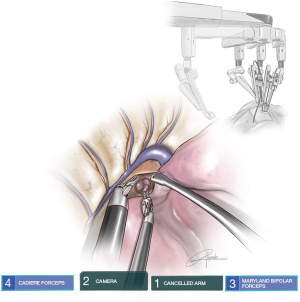
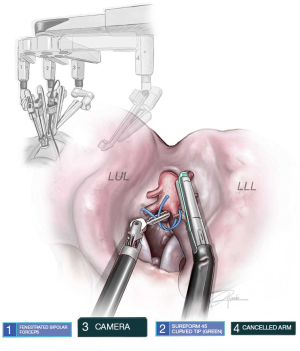
The da Vinci Xi system (Intuitive Surgical, Sunnyvale, CA, USA) is implanted through a single incision that is 2.5 cm in length, and the average length of the incision is between 3 and 4 cm. The incision is made in the 6th–7th intercostal (IC) area, between the anterior and mid-axillary lines (Figure 1). The robotic instruments and camera (30°) in the console represent the surgeon’s hands, wrists, and arms. The da Vinci Xi and X technologies have several ranges of movements. For optimal visibility, the table surgeon’s assistant should employ a long, curved suction, and the assistant plays a crucial role in the surgical planning for conversion procedures, as shown in Figure 2. The Da Vinci Xi system has 3D magnified high-definition video, which offers more precision than VATS, and it eliminates the physiological tremor. It also scales the movements, which can decrease the motions. When compared with VATS, the use of U-RATS’s specialized trocars, which allow staplers to be passed through them and into the chest, allows for greater maneuverability and requires fewer movements (Figure 3). During the procedure of dissecting lymph nodes, U-RATS have superior vision (Figure 4). The staplers have excellent access during the process of stapling the pulmonary vessels (Figure 5). In general, U-RATS have several advantages and disadvantages, as shown in Table 1.

Table 1
| Advantages of U-RATS |
| Cheaper (only 3 arms, no CO2, no guide, no adaptor for CO2, no need air seal) |
| Rapid docking, no need for targeting (1 min) |
| Less painful (single incision anterior approach) |
| Easy to undock in case of bleeding |
| Faster removal of staplers (with trocar) |
| Faster conversion to thoracotomy (enlarge the incision) |
| Easier than MRATS in case of strong adhesions (docking is difficult for MRATS in case of aspergilloma cases or TB) |
| Makes non-intubated technique more feasible and safer |
| 8 mm staplers will make it easier |
| Disadvantages of U-RATS |
| More demanding: assistant is 50% of surgery |
| Longer learning curve |
| Time consuming compared to U-VATS (more frequent the re-adaptation of arms, clearance, change trocar for staplers) |
| A set of long thoracoscopic instruments is needed (Scanlan international) |
| Utility incision is lower than U-VATS (more difficult for assistant) |
| In case of hybrid technique, assistant must be familiarized with U-VATS technique |
U-RATS, uniportal robotic-assisted thoracic surgery; MRATS, multi-portal robotic assisted thoracic surgery; TB, tuberculosis; U-VATS, uniportal video-assisted thoracoscopic surgery.
Complex resections
As compared to U-VATS, the U-RATS approach is superior for anatomic segmental resections, particularly those that include segments positioned more posteriorly. This is due to the fact that the robot enables more maneuverability and provides a deeper 3D view than U-VATS does. The robotic staplers have the largest angulation with good control by the surgeon, and the applicator of polymer ligating clips in U-RATS has an angulation of ninety degrees, which is more suitable for use during anatomic segmentectomies in the hands of an experienced surgeon (4).
A simpler anastomosis can be achieved with sleeve and bronchovascular resections when using the U-RATS technique. For the bronchial anastomosis, the most effective method is to make use of a barbed suture, and we recommend doing a running suture using one thread that is 35 centimeters long and two needles that are each 17 millimeters in size. Since we don’t risk losing tension when performing the anastomosis, this method of suturing is preferred in U-RATS for both reliability and safety. During the operation, it could be very challenging for the assistant to keep the tension up.
Another resection where U-RATS is very helpful is pneumonectomy, especially on the left side, not only for the 3D view but also for the angle of stapler insertion. We consider pneumonectomy by U-RATS more suitable than by U-VATS because the insertion of the stapler via the 6th or 7th ICS is easier with the robot helping to achieve a shorter stump of the bronchus.
The vital role of nurses in U-RATS approach
U-RATS is an innovative surgical technique that has been rapidly gaining popularity in recent years due to its various advantages over traditional open and thoracoscopic surgeries. One of the key factors contributing to the success of U-RATS is the critical role of nurses in the care of patients undergoing this procedure.
Firstly, the role of nurses in U-RATS begins even before the surgical procedure itself. During the preoperative phase, nurses work closely with the surgical team to prepare the patient for the procedure, including obtaining informed consent, conducting preoperative assessments, and ensuring that the patient is mentally and physically prepared for surgery. Nurses play a critical role in ensuring that the patient is adequately informed about the procedure, its benefits, and potential risks. They also assist in the administration of preoperative medications and prepare the patient for anesthesia.
During the intraoperative phase of U-RATS, nurses continue to play a vital role in ensuring the safety and well-being of the patient. They work closely with the surgeon and the anesthesiologist to monitor the patient’s vital signs and provide support during the procedure. Nurses are responsible for maintaining a sterile surgical environment, ensuring that all necessary equipment and instruments are available, and anticipating the needs of the surgical team. They are also responsible for documenting the surgical procedure accurately and communicating effectively with the surgical team.
Postoperatively, nurses continue to play a crucial role in the care of patients undergoing U-RATS. They monitor the patient’s vital signs, pain levels, and any signs of complications or adverse reactions to medications. Nurses are responsible for ensuring that the patient is comfortable and managing any postoperative pain. They also assist with the administration of medications, wound care, and patient education regarding postoperative care and discharge instructions.
In addition to their direct patient care responsibilities, nurses in U-RATS also play an important role in ensuring the quality and safety of the procedure. They assist in the development and implementation of protocols and guidelines for U-RATS, including the standardization of equipment and procedures. Nurses also participate in ongoing education and training programs to ensure that they are up-to-date with the latest advances in U-RATS and perioperative care.
The impact of nursing care on patient outcomes in U-RATS cannot be overstated. Several studies have demonstrated that high-quality nursing care is associated with improved patient outcomes, including a reduced length of hospital stay, decreased rates of postoperative complications, and improved patient satisfaction.
In conclusion, the role of nurses in U-RATS is critical and multifaceted, encompassing preoperative, intraoperative, and postoperative care. Nurses are indispensable members of the surgical team and play a crucial role in ensuring the safety, comfort, and well-being of patients undergoing this innovative surgical technique. Their impact on patient outcomes in U-RATS cannot be overstated, and ongoing education and training are essential to ensuring that nurses remain up-to-date with the latest advances in perioperative care.
Discussion
With the support of cutting-edge technology, the uniportal method has been rapidly progressing over the past decade. Since our team performed the world’s first U-VATS lobectomy in 2010 (5), we have refined the procedure for increasingly complex patients with the use of learned insight, streamlined tools, higher-definition cameras, and powered, more angular staplers (4). While we wait for this new robot to be validated for thoracic surgery, we have adopted to modify the Da Vinci Xi® in order to create the U-RATS technique, with the intention of carrying out the world’s first cases entirely handled by robotics in September of 2021 in Spain (4). Since then, we have improved the procedure and carried out all different kinds of resections, such as upper and lower segmentectomies, sleeves, dual sleeves, and carinal resections. We refer to robotic thoracic surgery that is performed through a single IC incision as pure “uniportal robotic-assisted thoracic surgery” (U-RATS). This type of robotic thoracic surgery does not involve the spreading of ribs and makes use of a robotic camera, robotic dissecting instruments, and robotic staplers.
In January 2022, we published the study that described the pure U-RATS aspects, techniques, and recommendations for U-RATS (4). In October 2022 in Italy, Vincenzi et al. reported 2 cases that underwent the U-RATS approach (6). To date, we have successfully completed more than 140 cases including also sleeves, double sleeves, segmentectomies, complex lobectomies and carinal resections (4,7-10). Currently, only a few thoracic surgeons performed and experienced with U-RATS approach (4,6-8,11-14). Recently, a video tutorial was recorded in UK with Joel Dunning, “A Step-by-Step Guide to Setup” where there is important information about this method for installing the ports and arranging the arms in such a way as to prevent the robotic system from accidentally colliding with one another (10,11).
However, Melfi et al. (15) reported the first series of pulmonary lobectomies that were done via robot assisted approach with the Da Vinci System. It composes of four-arm approach; 3 cm utility port in the 4th–5th ICS with the right robotic arm, a camera port in the 7th–8th ICS mid-axillary line, a robotic left port in the 6th–7th ICS posterior axillary line, and the assistant port between utility and camera port (16). Wilson and Boffa in their study explained that robotic techniques have more levels in nodal upstaging than VATS in stage 1 non-small cell lung cancer (17,18).
Robotic assisted thoracic surgery has better vision, more static movement, higher maneuverability and more capability during lymph node dissection than U-VATS nowadays (19), there are difficulties for subcarinal (station 7), especially during left U-VATS, but U-RATS has excellent access, and U-RATS approach is applicable to patients with a small thoracic cavity who have narrow ICS (2). When compared to the traditional open and multiport methods, the single incision method has been shown to reduce postoperative pain and speed up the patient’s return to normal life, even in the most complex of cases (20-25). The first U-VATS lobectomy in the world was done by Diego’s group in 2010 (5). Since that time, the uniportal approach is developing rapidly and complex cases can be performed easily (4,26-30). Thoracoscopy via uniportal incision has less postoperative pain and more rapid recovery (31).
The robotic-assisted thoracic surgery known as the Pure U-RATS is performed through a single IC incision and does not include the dispersal of ribs. The robotic camera, robotic dissecting equipment, and robotic staplers are all utilized throughout the procedure (4). Via a single port robotic platform in the cadaveric model, Gonzalez-Rivas et al. (8) progressed the technique of lobectomy and thymectomy through subxiphoid and subcostal approaches in 2018 (4). The instruments and arms during uniportal approach should be placed in a specific way not to cause collision (7).
The robotic-assisted carinal resections were performed through a multiport approach (4,5). But with the evolution of the U-RATS technique, the complex carinal resection and reconstruction can be done safely and feasibly (7). Carinal resection and reconstruction are difficult and challenging surgeries even with thoracotomy, and they have dangerous complications even if they will be done by expert thoracic surgeons (32).
The robotic technology has excellent 3D view and precision, and it decreases complications of tracheal surgery like extensive dissection, which causes devascularization, tensions during anastomosis, and not free margins (33).
In the year 2021, Yang and his colleagues detailed a procedure for executing a right upper lobectomy utilizing the Da Vinci Robotic Surgery System Xi®, which was completed by devices built specifically for the VATS technique. This approach required only a single incision (dissector, grasper, suction, and staplers). They called this method a hybrid U-RATS-VATS approach (34). Hybrid technique with uniportal approach by using both VATS and U-RATS is different: the incision is placed as in U-VATS (4th–5th ICS), with robotic arms set-up as in U-RATS. During stapling, the VATS staplers are inserted by the assistant (who must be master in the uniportal technique). The assistant surgeon must be skillful, well-trained, and conversant with the tools (4). Because the surgeon needs to rely on the assistance for the tough parts of the procedure, we don’t advise using a U-RATS-VATS combination; although, if any thoracic surgeon wants to do the hybrid uniportal technique, we were of the opinion that it would be more beneficial to remove the robotic arms in order to obtain additional space for the insertion of the stapler. The comparison of both U-VATS and U-RATS has been explained in (Table 2). In terms of feasibility, safety, oncological outcomes, and the postoperative recovery period, the pure uniportal approach utilizing robotic technology would be a significant improvement. In patients with lung cancer, RATS provides an excellent lymph node dissection and offers the best prognosis (2-4).
Table 2
| Items labeled | U-VATS | U-RATS |
|---|---|---|
| (I) The incision place | 4th–5th intercostal space, a little anterior to the mid-axillary lines | 6th–7th intercostal space, just anterior to the mid-axillary lines |
| (II) Using of wound retractor | Has benefit. If not used, cleaning of the camera is frequently used | Mandatory if missed, cleaning of the camera is repeatedly needed, which needs more time for repositioning of the camera from the trocar |
| (III) Scopes with camera angles | 30 degrees | 30 degrees |
| (IV) Thoracoscopic devices | VATS type. Camera. Grasper. Dissection. Stapler. Suction | Three robotic arms. Camera. Holding. Working/stapler. 2 VATS tools: longer and more curved suction and grasper (subxiphoid length) |
| (V) Entrance into the thorax (e.g., during strong adhesions) | Hard during removal of adhesion in the surrounding areas of the wound retractor | Hard during removal of adhesion in the surrounding areas of the wound retractor |
| (VI) Leaning of the table | It is required which gives more and better view | It is not required |
| (VII) Dissection of mediastinal lymph nodes | All stations are reachable but for subcarinal (station 7) has less access especially during left U-VATS | All stations are accessible. Excellent manoeuvrability. It has fewer difficulties |
| (VIII) Bleeding control | For bleeding control; easily and quickly can be converted to open. Standardized by practice and international expert consensus (25) | When bleeding was not controlled by U-RATS, undocking is quick and conversion to U-VATS or thoracotomy is rapidly performed |
| (IX) Anaesthesia with single-lung ventilation | Heavily required. It can be done with Intermittent ventilation. In some elected cases tubeless technique can be used | The operation should be performed under general anaesthesia with single-lung ventilation |
| (X) Assistant help | Must have skill. Holding the camera. Exposure | Skill demanding, must follow the surgeon’s movements. VATS tools can be used via the assistant between the robotic arms |
U-VATS, uniportal video-assisted thoracoscopic surgery; U-RATS, uniportal robotic-assisted thoracic surgery.
Limitations of using U-RATS
Robotic surgery has some drawbacks, such as its high upfront costs, prolonged setup time, inability to palpate the lung, and absence of haptic feedback (35,36). Cardiothoracic and vascular surgeons should have extensive experience with the robot and be well-versed in U-VATS procedures; however, their lack of familiarity with U-VATS is the primary barrier. When compared to M-RATS, the U-RATS instrumentation has fewer chances of accidental collisions. We suggest switching to B-RATS before beginning U-RATS, after the initial phase of M-RATS has been completed. We suggest that surgeons performing B-RATS make an incision in the 5th ICS and another in the 7th ICS. Similarly, to U-VATS, the camera must be positioned at the top of the incision, and instruments inserted into the bottom of the incision and the accessory port are used to triangulate and complete the procedure. To achieve the necessary level of proficiency in U-RATS, a surgeon must first be an expert in U-RATS and have some prior experience with M-RATS and, should gain competence with the biportal robotic approach.
To avoid instrument collisions in U-RATS, their movements must be different from those of M-RATS, which adds time to the surgical process while the surgeon learns how to use the system. The surgeon’s assistant needs to be an expert in the uniportal access method. It is challenging to use robotic staplers during lobectomy if the incision is too high, and it is also difficult for the assistant to move around if the incision is too low. In order to increase the amount of space available, trocars with a diameter of 8 millimeters are inserted via the single incision made for the dissection. When it comes time to staple, however, the anterior trocar should be replaced with a 12-millimeter trocar.
Conclusions
The U-RATS offers excellent maneuverability, accessibility and deeper 3D view compared with a thoracoscopic single port approach. The more precise robotic equipment makes it easier to separate distant anatomical parts and remove intrapulmonary lymph nodes located deeper in the lung. For sleeve and bronchovascular resections the U-RATS approach makes easier the anastomosis. Through a single anterior incision, U-RATS brings the benefits of robotic staplers, protecting delicate blood vessel walls from the harsh, uneven movement that can occur when using VATS staplers in less-than-expert hands. Nurses are indispensable members of the surgical team and play a crucial role in ensuring the safety, comfort, and well-being of patients undergoing this innovative surgical technique. Their impact on patient outcomes in U-RATS cannot be overstated, and ongoing education and training are essential to ensuring that nurses remain up-to-date with the latest advances in perioperative care.
Acknowledgments
The authors acknowledge their respective universities/institutes/organizations.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Carlos Galvez Munoz and Paula A. Ugalde Figueroa) for the series “Advanced Uniportal VATS” published in Video-Assisted Thoracic Surgery. The article has undergone external peer review.
Peer Review File: Available at https://vats.amegroups.com/article/view/10.21037/vats-22-54/prf
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://vats.amegroups.com/article/view/10.21037/vats-22-54/coif). The series “Advanced Uniportal VATS” was commissioned by the editorial office without any funding or sponsorship. DGR serves as an unpaid editorial board member of Video-Assisted Thoracic Surgery from August 2021 to July 2023. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lin J. Robotic lobectomy: revolution or evolution? J Thorac Dis 2017;9:2876-80. [Crossref] [PubMed]
- Manolache V, Motas N, Bosinceanu ML, et al. Comparison of uniportal robotic-assisted thoracic surgery pulmonary anatomic resections with multiport robotic-assisted thoracic surgery: a multicenter study of the European experience. Ann Cardiothorac Surg 2023;12:102-9. [Crossref] [PubMed]
- Paradela M, Garcia-Perez A, Fernandez-Prado R, et al. Uniportal robotic versus thoracoscopic assisted surgery: a propensity score-matched analysis of the initial 100 cases. Ann Cardiothorac Surg 2023;12:23-33. [Crossref] [PubMed]
- Gonzalez-Rivas D, Manolache V, Bosinceanu ML, et al. Uniportal pure robotic-assisted thoracic surgery—technical aspects, tips and tricks. Ann Transl Med 2022; [Crossref]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Vincenzi P, Lo Faso F, Eugeni E, et al. Uniportal robotic-assisted thoracoscopic surgery for early-stage lung cancer with the Da Vinci Xi: Initial experience of two cases. Int J Med Robot 2023;19:e2477. [Crossref] [PubMed]
- Gonzalez-Rivas D, Essa RA, Motas N, et al. Uniportal robotic-assisted thoracic surgery lung-sparing carinal sleeve resection and reconstruction. Ann Cardiothorac Surg 2023;12:130-2. [Crossref] [PubMed]
- Gonzalez-Rivas D, Ismail M. Subxiphoid or subcostal uniportal robotic-assisted surgery: early experimental experience. J Thorac Dis 2019;11:231-9. [Crossref] [PubMed]
- Gonzalez Rivas D, Manolache V, Bosinceanu M, et al. Uniportal Pure Robotic-Assisted Thoracic Surgery—Left Bisegmentectomy S9-S10. CTSNet. 2022 [cited 2022 Dec 3]. Available online: https://www.ctsnet.org/article/uniportal-pure-robotic-assisted-thoracic-surgery—left-bisegmentectomy-s9-s10
- Gonzalez Rivas D, Bosinceanu M, de Oliveira HA, et al. Uniportal Robotic Left Upper Lobe Sleeve Resection. CTSNet. 2022 [cited 2022 Dec 3]. Available online: https://www.ctsnet.org/article/uniportal-robotic-left-upper-lobe-sleeve-resection
- Gonzalez-Rivas D, Bosinceanu M, Motas N, et al. Uniportal robotic-assisted thoracic surgery for lung resections. Eur J Cardiothorac Surg 2022;62:ezac410. [Crossref] [PubMed]
- Mercadante E, Martucci N, De Luca G, et al. Early experience with uniportal robotic thoracic surgery lobectomy. Front Surg 2022;9:1005860. [Crossref] [PubMed]
- Gonzalez Rivas D, Bosinceanu M, Dunning J. The New Era of Uniportal Robotic Surgery: An Interview with Diego Gonzalez Rivas. CTSNet. 2022 [cited 2022 Dec 3]. Available online: https://www.ctsnet.org/article/new-era-uniportal-robotic-surgery-interview-diego-gonzalez-rivas
- Dunning J, Waterhouse B, Gonzalez Rivas D. The UK’s First Uniportal Robotic Surgery with Diego Gonzales Rivas. CTSNet. 2022 [cited 2022 Dec 3]. Available online: https://www.ctsnet.org/article/uks-first-uniportal-robotic-surgery-diego-gonzales-rivas
- Melfi FM, Menconi GF, Mariani AM, et al. Early experience with robotic technology for thoracoscopic surgery. Eur J Cardiothorac Surg 2002;21:864-8. [Crossref] [PubMed]
- Parini S, Massera F, Papalia E, et al. Port Placement Strategies for Robotic Pulmonary Lobectomy: A Narrative Review. J Clin Med 2022;11:2612. [Crossref] [PubMed]
- Wilson JL, Louie BE, Cerfolio RJ, et al. The prevalence of nodal upstaging during robotic lung resection in early stage non-small cell lung cancer. Ann Thorac Surg 2014;97:1901-6; discussion 1906-7. [Crossref] [PubMed]
- Boffa DJ, Kosinski AS, Paul S, et al. Lymph node evaluation by open or video-assisted approaches in 11,500 anatomic lung cancer resections. Ann Thorac Surg 2012;94:347-53; discussion 353. [Crossref] [PubMed]
- Hirpara DH, Kidane B. Commentary: VATS, RATS, stats, and some caveats. J Thorac Cardiovasc Surg 2021;162:269-70. [Crossref] [PubMed]
- Gonzalez-Rivas D, Bosinceanu M, Manolache V, et al. Uniportal fully robotic-assisted major pulmonary resections. Ann Cardiothorac Surg 2023;12:52-61. [Crossref] [PubMed]
- Ning Y, Chen Z, Zhang W, et al. Uniportal three-arm robotic-assisted thoracic surgery right upper lobe and carinal sleeve resection. Ann Cardiothorac Surg 2023;12:70-2. [Crossref] [PubMed]
- Wang R, Gonzalez-Rivas D, Wang C, et al. Non-intubated uniportal robotic-assisted thoracic surgery: the future of thoracic surgery? Ann Cardiothorac Surg 2023;12:49-51. [Crossref] [PubMed]
- Gonzalez-Rivas D, Bale M, Bosinceanu ML, et al. Uniportal robotic-assisted thoracoscopic surgery right upper lobectomy for aspergilloma. Ann Cardiothorac Surg 2023;12:142-3. [Crossref] [PubMed]
- Gonzalez-Rivas D, Koziej PH, Sediqi S, et al. Uniportal hybrid robotic-assisted right upper sleeve lobectomy in an 83-year-old patient with severe pulmonary hypertension. Ann Cardiothorac Surg 2023;12:136-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Bosinceanu M, Manolache V, et al. Uniportal fully robotic-assisted bronchovascular sleeve bilobectomy. Ann Cardiothorac Surg 2023;12:144-6. [Crossref] [PubMed]
- Essa RA, Ahmed SK, Bapir DH. Uniportal video-assisted thoracoscopic right lower and middle sleeve bilobectomy for a neglected carcinoid tumor. Ann Med Surg (Lond) 2022;75:103359. [Crossref] [PubMed]
- Ahmed SK, Essa RA, Bapir DH. Uniportal Video-assisted Thoracoscopic Surgery (u-VATS) for Management of pulmonary hydatid cyst: A systematic review. Ann Med Surg (Lond) 2022;75:103474. [Crossref] [PubMed]
- Essa RA, Ahmed SK, Mohamed MG. Pulmonary hydatid cyst mimicking lung tumor in a heavy smoker patient- Uniportal VATS management. Int J Surg Case Rep 2022;95:107138. [Crossref] [PubMed]
- Essa RA, Ahmed SK. Life-Threatening Cardiac Tamponade Secondary to COVID-19 Treated with Uniportal Video-Assisted Thoracoscopic Surgery: A Case Report. Am J Case Rep 2022;23:e935839. [Crossref] [PubMed]
- Essa RA, Ahmed SK, Bapir DH. Uniportal video-assisted thoracoscopic surgery (UVATS) right lower lobectomy for a giant T4 squamous cell lung tumour. J Int Med Res 2022;50:3000605221097374. [Crossref] [PubMed]
- Magouliotis DE, Fergadi MP, Spiliopoulos K, et al. Uniportal Versus Multiportal Video-Assisted Thoracoscopic Lobectomy for Lung Cancer: An Updated Meta-analysis. Lung 2021;199:43-53. [Crossref] [PubMed]
- Grillo HC. Carinal reconstruction. Ann Thorac Surg 1982;34:356-73. [Crossref] [PubMed]
- Hu D, Wang Z, Tantai J, et al. Robotic-assisted thoracoscopic resection and reconstruction of the carina. Interact Cardiovasc Thorac Surg 2020;31:912-4. [Crossref] [PubMed]
- Yang Y, Song L, Huang J, et al. A uniportal right upper lobectomy by three-arm robotic-assisted thoracoscopic surgery using the da Vinci (Xi) Surgical System in the treatment of early-stage lung cancer. Transl Lung Cancer Res 2021;10:1571-5. [Crossref] [PubMed]
- Cerfolio RJ. Total port approach for robotic lobectomy. Thorac Surg Clin 2014;24:151-6. v. [Crossref] [PubMed]
- Soliman BG, Nguyen DT, Chan EY, et al. Impact of da Vinci Xi robot in pulmonary resection. J Thorac Dis 2020;12:3561-72. [Crossref] [PubMed]
Cite this article as: Essa RA, Ahmed SK, Bale M, Bosinceanu ML, Gallego Poveda J, Garcia-Perez A, Gonzalez-Rivas D. Challenges for pure uniportal robotic-assisted thoracoscopic surgery. Video-assist Thorac Surg 2023;8:18.