Returning to baseline daily ambulation after cardiothoracic surgery
Highlight box
Key findings
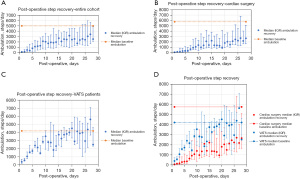
• For cardiac surgery and VATS patients, there is a strong positive correlation between increasing post-operative day and daily number of steps. Cardiac surgery patients return to pre-operative ambulation levels at post operative day 26 and VATS patients return to pre-operative ambulation levels at post-operative day 9.
What is known and what is new?
• Functional recovery is an important metric post-operatively as immobility is associated with post-operative complications. Post-operative walking trajectories predict risk of delirium and hospital readmission.
• This data describes the post-operative walking recovery after cardiac surgery and VATS in a cohort of patients at a Veterans Health Administration hospital.
What is the implication, and what should change now?
• After cardiac surgery and VATS, ambulatory recovery should be linear. Post-operative number of steps can now be easily monitored with wearable smart devices. Deviation of a linear walking recovery should raise concern of possible complications.
Introduction
Prolonged immobility after surgery leads to complications including insulin resistance, deconditioning, venous thromboembolism, pulmonary complications and delirium (1-4). Enhanced recovery after surgery (ERAS) and enhanced recovery after thoracic surgery (ERATS) pathways have focused on early ambulation to reduce these complications and improve postoperative metrics such as inpatient length of stay in abdominal, thoracic and cardiac surgeries (1,4,5). Despite the well described benefits of early ambulation, there are few studies that objectively assess post-operative ambulation recovery and those which do are limited to only inpatient measurements (6). Information regarding trajectories of post-operative ambulation recovery and return to baseline walking would allow surgeons to better counsel patients regarding their functional recovery after surgery.
As ambulatory data have become readily available with the growing popularity of smart devices, it can be utilized by patients and clinicians to quantify mobility recovery after major operations. Furthermore, walking trends have even been shown to be relevant in predicting risk of readmission (7). The purpose of this study was to describe and quantify post-operative walking recovery data for 4 weeks post-operatively in patients undergoing video-assisted thoracoscopic surgery (VATS) and open cardiac operations. Following VATS and open cardiac surgery, we anticipated a linear post-operative walking recovery for both VATS and cardiac surgery patients and a sooner return to pre-operative baseline for those undergoing VATS than cardiac surgery as a nature of the operations. We present the following article in accordance with the STROBE reporting checklist (available at https://vats.amegroups.com/article/view/10.21037/vats-22-24/rc) (8).
Methods
This is a single-institution, prospective cohort study of patients undergoing elective cardiac and thoracic operations during a 3-year enrollment period (September 2016 through August 2019). Adults seen in clinic were screened if they were undergoing either an elective VATS operation or an elective cardiac operation at the Rocky Mountain Regional Veterans Affairs Medical Center during the study period. Exclusion criteria included those who did not walk at baseline and those not undergoing elective operations as pre-operative walking data could not be gathered. Participants without ≥3 days of pre-operative walking data or the full 28 days of post-operative walking data (including those lost to follow-up) were not included in analysis. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All participants provided written informed consent before participation and the study has obtained Clinical Research Ethics Committee approval (Colorado Multi-Institutional Review Board approval #16-1776).
At their pre-operative visit, participants that were recruited were provided with and instructed to wear a commercially available activity monitoring wristband (Vivofit3; Garmin Ltd, Schaffenhausen, Switzerland) on their nondominant wrist. The activity tracker is validated to track steps with <1% deviation from the gold standard of video observation (9). Baseline daily steps were recorded for 3 to 10 consecutive days pre-operatively. The day of surgery, walking data was not collected and the activity monitor was kept with the patients’ personal belongings. Post-operatively, daily steps were recorded for 28 consecutive days, beginning on post-operative day 1 regardless of disposition (intensive care, floor, or home). Patients wore the activity monitor continuously. Data from the activity tracker were downloaded for each participant using the commercially available wireless USB ANT Stick (Garmin Ltd) on the day of surgery and at their post-operative visit. Devices were synced with software updates at minimum once per month during the study period.
Preoperative baseline number of steps per day was reported by calculating the median steps for all days measured preceding surgery. Post-operative steps were expressed in absolute numbers and as percentages of preoperative baseline median. Patient data recorded included demographic information, comorbidities, surgery performed, operation duration, post-operative day 1 pain rating and total hospital length of stay. To minimize bias in comparison of subgroups, baseline demographics and comorbidities which may affect post-operative ambulation between groups were compared. Furthermore, pre-operative number of steps between groups were also compared.
Microsoft Excel (Microsoft, Redmond, WA, USA) and the R Project for Statistical Computing Version 4.2.1 (The R Foundation, Vienna, Austria) were used for data management and analysis. Steps per day on post-operative day 1 and post-operative day 28 were compared between those undergoing VATS and cardiac surgery using a Wilcoxon rank-sum test. Correlation analysis was performed using the Spearman correlation coefficient for post-operative day and the number of steps per day for the entire cohort and for each of the two operative categories. Increase in steps for each week post-operatively was used to determine the period of greatest ambulation recovery and compared between operative categories. Lastly, steps taken on each post-operative day was used to determine each patient’s return to pre-operative ambulation. P values <0.05 were considered significant.
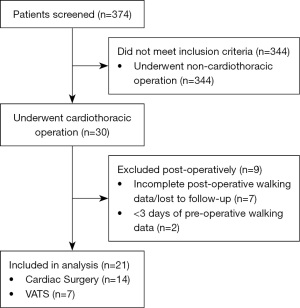
Results
During the 3-year enrollment period, 374 patients were screened for the study; 30 patients were enrolled and underwent VATS or cardiac surgery in the designated period, although 7 were lost to follow-up and 2 had incomplete pre-operative walking data. There were 21 patients included in analysis with complete 3–10 days of pre-operative and 28 days of post-operative walking data. The participant enrollment diagram is presented in Figure 1. Baseline demographics are described in Table 1. Univariate analysis demonstrated statistical difference for pre-operative hypertension (P=0.05), operating room time (P=0.02) and hospital length of stay (P=0.001) between those undergoing VATS and cardiac surgery. For the entire cohort, median (25th–75th percentile) baseline preoperative ambulation was 4,985 (3,154–7,109) steps/day with no difference between VATS and cardiac surgery cohorts (P=0.32).
Table 1
| Attribute | Total cohort (n=21) | Cardiac surgery (n=14) | VATS (n=7) | P value |
|---|---|---|---|---|
| Baseline demographics | ||||
| Age (years), mean ± SD | 66±11 | 66±11 | 67±12 | 0.92 |
| Male sex, n [%] | 20 [95] | 14 [100] | 6 [86] | 0.16 |
| Body mass index (kg/m2), (25–75%) | 30 [29–33] | 30 [29–33] | 29 [28–30] | 0.11 |
| Body surface area (m2), mean ± SD | 2.1±0.3 | 2.2±0.3 | 2.1±0.2 | 0.39 |
| New York Heart Association Heart Failure Classification, (25–75%) | 2 [1–3] | 2 [1–3] | 2 [1–3] | >0.99 |
| EuroSCORE II (%), (25–75%) | N/A | 1.7 (0.9–3.4) | N/A | N/A |
| Diabetes, n [%] | 4 [19] | 4 [29] | 0 | 0.13 |
| COPD, n [%] | 3 [14] | 3 [21] | 0 | 0.20 |
| Hypertension, n [%] | 6 [29] | 6 [43] | 0 | 0.05* |
| Intraoperative metrics | ||||
| Operating room time (min), (25–75%) | 274 [204–373] | 329 [240–404] | 195 [142–260] | 0.02* |
| Post-operative metrics | ||||
| POD #1 pain rating† (25–75%) | 4 [4–7] | 4 [4–7] | 5 [4–7] | >0.99 |
| Hospital length of stay‡ (days), (25–75%) | 7 [6–9] | 9 [7–10] | 4 [3–5] | 0.001* |
*, statistically significant (P<0.05); †, numerical rating scale [0–10] was used for post-operative day #1 pain rating; ‡, hospital length of stay was defined as number of midnights a patient was in the hospital. VATS, video assisted thoracoscopic surgery; SD, standard deviation; N/A, not applicable; COPD, chronic obstructive pulmonary disease; POD, post-operative day.
Seven patients (33%) underwent VATS and 14 (67%) underwent cardiac surgery. Operations performed via VATS included pulmonary resection (n=5, 24%), pleurodesis (n=1, 5%) and diaphragm plication (n=1, 5%). Cardiac surgeries included coronary artery bypass grafting (CABG) (n=4, 19%), aortic valve replacement (AVR) (n=3, 14%), combination cardiac procedures (hemiarch/CABG or AVR/CABG n=3, 14%), mitral valve replacement (n=2, 10%) and hemiarch replacement (n=2, 10%). On post-operative day 1, those who underwent VATS walked more steps than those who underwent cardiac surgery as shown in Table 2 (P=0.02). By post-operative day 28, there was no statistical difference in number of steps between the two cohorts, also shown in Table 2 (P=0.91).
Table 2
| Time | Cardiac surgery (n=14) | VATS (n=7) | P value |
|---|---|---|---|
| Pre-operative baseline | |||
| Median steps/day (25–75%) | 5,741 [3,602–7,913] | 4,197 [2,716–5,535] | 0.32 |
| Post-operative day #1 | |||
| Median steps/day (25–75%) | 53 [0–120] | 393 [184–703] | 0.02* |
| % pre-operative level | 1 | 9 | |
| Post-operative day #28 | |||
| Median steps/day (25–75%) | 2,654 [1,641–5,103] | 2,511 [2,312–4,607] | 0.91 |
| % pre-operative level | 46 | 60 | |
| Week 1 step recovery | |||
| Increase in steps/day | 133 | 272 | 0.05* |
| % Increase in steps/day† | 2 | 6 | |
| Week 2 step recovery | |||
| Increase in steps/day | 100 | 190 | 0.50 |
| % Increase in steps/day† | 2 | 4 | |
| Week 3 step recovery | |||
| Increase in steps/day | −3 | 108 | 0.25 |
| % Increase in steps/day† | 0 | 2 | |
| Week 4 step recovery | |||
| Increase in steps/day | 205 | −144 | 0.03* |
| % Increase in steps/day† | 4 | −3.2 |
†, percent as a function of pre-operative baseline steps/day; *, statistically significant (P<0.05). VATS, video assisted thoracoscopic surgery.
For the entire cohort, and VATS and cardiac surgery independently, there was a positive correlation between daily number of steps and post-operative days (P<0.001), described in Table 3 and demonstrated visually in Figure 2A-2C. Ambulatory recovery for patients who underwent VATS was significantly greater in week 1 than those who underwent cardiac surgery (P=0.05) while ambulatory recovery for those who underwent cardiac surgery was significantly greater in week 4 than those who underwent VATS (P=0.03), demonstrated in Table 2. There was no statistical difference in step recovery between the groups in weeks 2 or 3, also shown in Table 2. There was no statistical difference from baseline on post-operative day 9 for those who underwent VATS which continued for the remainder of the 28 days evaluated. There was no statistical difference from baseline on post-operative day 26 for those who underwent cardiac surgery, although statistical significance returned for post-operative days 27 and 28. To allow for visual comparison of ambulatory recovery between cardiac surgery and VATS patients, the recovery trajectories are combined in Figure 2D.
Table 3
| Metric | Total cohort (n=21) | Cardiac surgery (n=14) | VATS (n=7) |
|---|---|---|---|
| Spearman correlation coefficient | 0.853 | 0.894 | 0.804 |
| P value | <0.001* | <0.001* | <0.001* |
*, statistically significant (P<0.05). VATS, video assisted thoracoscopic surgery.
Discussion
This study describes the overall ambulation recovery trends for two approaches to intrathoracic surgery: VATS and cardiac surgery. There is a strong positive correlation for increasing number of daily steps with increasing post-operative day in both cohorts. While there was a statistically significant difference in post-operative number of steps on post-operative day 1 for those who underwent VATS as compared to those who underwent cardiac surgery, by post-operative day 28, there was no difference in number of steps between the groups. Figure 2D allows for visual comparison of recovery trajectory between subgroups and there is a clear discordance in ambulation during week 1, although number of steps converge visually thereafter. This is likely due to a nature of the operation including invasiveness and requirement of cardiopulmonary bypass in the cardiac surgery group, which initially impacts ambulatory recovery in the immediate post-operative setting. Additionally for VATS patients, there was no difference between number of steps per day compared to baseline on post-operative day 9. On post-operative day 27, the median number of steps for VATS patients exceeds baseline (Figure 2C). Although this single day appears much higher, it is within the expected day to day variation. Patients who underwent cardiac surgery recovered later post-operatively with peak increase in steps per day during week 4, which was higher than week 4 recovery of VATS patients.
Walking data are clinically useful as ambulation serves as a measure of functional status, which is related to overall wellness (10-12). Prior work demonstrates the relationship of functional status with overall health, including recovery in the post-operative setting (1,5,13-15). Individual walking data is ubiquitous with increased popularity of activity tracker devices and can now be used by surgeons and patients alike to better understand postoperative recovery (16). This provides patients with information regarding their expected post-operative functional recovery, allowing them to plan accordingly.
For clinicians, ambulatory data available on a patient’s smart device may allow them to be benchmarked to the cohort presented here. Furthermore, deviation from the expected recovery may put patients at risk for the known complications of reduced post-operative ambulation. It is feasible that future clinicians could monitor daily ambulation remotely to look for deviations or lagging from the sample described here. Currently, post-operative walking data has proven successful in risk stratification for post-operative delirium and readmission (3,7). In order to use walking trends to predict other complications such as insulin resistance, venous thromboembolism, pulmonary complications, and prolonged inpatient length of stay, general post-operative ambulatory trends must be described.
The limitations of this study include sample size and duration of follow-up. The relatively low volume of cardiac patients provided a small number of participants and subsequently, patients were eliminated from analysis due to incomplete data collection (<28 days post-operatively). Similarly, most of the patients were male due to the demographics within the patients treated at the Veteran Health Administration Hospital. The small number of participants and skewed sex enrollment may subject this study to bias. Despite this, the number of participants is similar to prior work describing ambulation after cardiac surgery and baseline attributes which may impact post-operative ambulatory recovery were compared in Table 1 (6). The variation in ambulation of different populations is well established, although the population presented here mobilize adequately (11,17). Notably, data were collected for 28 days post-operatively, yet this did not capture true return to baseline for cardiac surgery patients as there remains a statistical difference in number of steps from pre-operative baseline on post-operative days 27 and 28. Future studies should follow cardiac surgery patients for longer post-operatively, although their prolonged recovery time may also be related to the prolonged hospitalization as compared with VATS patients (P=0.001, Table 1). Lastly, the Vivofit 3 used in this study only measures number of steps and cannot quantify stationary activity such as laying, sitting or standing, which may be notable to quantify in the immediate post-operative setting (6). The Vivofit 3 also cannot differentiate walking from running or record other non-stationary activity such as swimming or bicycling, which would be relevant in post-operative functional recovery. Future studies may consider a wearable device which can measure a multitude of stationary and non-stationary activities.
Conclusions
Recovery of post-operative ambulation after VATS and cardiac surgery is directly related to increasing post-operative day. VATS patients have an early ambulatory recovery peaking in week 1 and ambulation is without statistical difference from preoperative baseline levels by post-operative day 9. Patients undergoing cardiac surgery have a later ambulatory recovery peaking in week 4 and ambulation is without statistical difference from baseline by post-operative day 26. Further work should include a larger sample size and longer duration of ambulation data for patients undergoing cardiac surgery. This information can be used to counsel patients about expected post-operative activity recovery.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Mark R. Katlic) for the series “VATS in Older Adults” published in Video-Assisted Thoracic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://vats.amegroups.com/article/view/10.21037/vats-22-24/rc
Data Sharing Statement: Available at https://vats.amegroups.com/article/view/10.21037/vats-22-24/dss
Peer Review File: Available at https://vats.amegroups.com/article/view/10.21037/vats-22-24/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://vats.amegroups.com/article/view/10.21037/vats-22-24/coif). The series “VATS in Older Adults” was commissioned by the editorial office without any funding or sponsorship. RAM serves as an unpaid editorial board member of Video-Assisted Thoracic Surgery from July 2022 to June 2024. RAM reports that he is the PI on an AHRQ R01 grant, 1R01HS027417-01A1, for which he received salary support paid to his institution then reimbursed to him. The focus of this grant is unrelated to the project authors have submitted for consideration of publication; RAM also reports he is a consultant for Medtronic and received salary support paid to his institution then reimbursed to him. The nature of this consultancy is unrelated to the project authors have submitted for consideration of publication. ELJ reports that he received Consulting Fees for teaching Lap CBDE Courses from Boston Scientific and Payment for record review from James Caviola and Harvard RMF. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All participants provided written informed consent before participation and the study has obtained Clinical Research Ethics Committee approval (Colorado Multi-Institutional Review Board approval #16-1776).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hu Y, McArthur A, Yu Z. Early postoperative mobilization in patients undergoing abdominal surgery: a best practice implementation project. JBI Database System Rev Implement Rep 2019;17:2591-611. [Crossref] [PubMed]
- Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;55:91-115. [Crossref] [PubMed]
- Robinson TN, Kovar A, Carmichael H, et al. Postoperative delirium is associated with decreased recovery of ambulation one-month after surgery. Am J Surg 2021;221:856-61. [Crossref] [PubMed]
- Moradian ST, Najafloo M, Mahmoudi H, et al. Early mobilization reduces the atelectasis and pleural effusion in patients undergoing coronary artery bypass graft surgery: A randomized clinical trial. J Vasc Nurs 2017;35:141-5. [Crossref] [PubMed]
- Carmichael JC, Keller DS, Baldini G, et al. Clinical Practice Guidelines for Enhanced Recovery After Colon and Rectal Surgery From the American Society of Colon and Rectal Surgeons and Society of American Gastrointestinal and Endoscopic Surgeons. Dis Colon Rectum 2017;60:761-84. [Crossref] [PubMed]
- Halfwerk FR, van Haaren JHL, Klaassen R, et al. Objective Quantification of In-Hospital Patient Mobilization after Cardiac Surgery Using Accelerometers: Selection, Use, and Analysis. Sensors (Basel) 2021;21:1979. [Crossref] [PubMed]
- Robinson TN, Carmichael H, Hosokawa P, et al. Decreases in daily ambulation forecast post-surgical re-admission. Am J Surg 2022;223:857-62. [Crossref] [PubMed]
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344-9. [Crossref] [PubMed]
- Höchsmann C, Knaier R, Eymann J, et al. Validity of activity trackers, smartphones, and phone applications to measure steps in various walking conditions. Scand J Med Sci Sports 2018;28:1818-27. [Crossref] [PubMed]
- Lee IM, Buchner DM. The importance of walking to public health. Med Sci Sports Exerc 2008;40:S512-8. [Crossref] [PubMed]
- Tudor-Locke C, Bassett DR Jr. How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med 2004;34:1-8. [Crossref] [PubMed]
- Nauman J, Khan MAB, Joyner MJ. Walking in the Fast Lane: High-Intensity Walking for Improved Fitness and Health Outcomes. Mayo Clin Proc 2019;94:2378-80. [Crossref] [PubMed]
- Schujmann DS, Teixeira Gomes T, Lunardi AC, et al. Impact of a Progressive Mobility Program on the Functional Status, Respiratory, and Muscular Systems of ICU Patients: A Randomized and Controlled Trial. Crit Care Med 2020;48:491-7. [Crossref] [PubMed]
- Shay A, Fulton JS, O'Malley P. Mobility and Functional Status Among Hospitalized COPD Patients. Clin Nurs Res 2020;29:13-20. [Crossref] [PubMed]
- Adogwa O, Elsamadicy AA, Fialkoff J, et al. Early Ambulation Decreases Length of Hospital Stay, Perioperative Complications and Improves Functional Outcomes in Elderly Patients Undergoing Surgery for Correction of Adult Degenerative Scoliosis. Spine (Phila Pa 1976) 2017;42:1420-5. [Crossref] [PubMed]
- MejiaCruz Y. Walking speed measurement technology: A review. Curr Geriatr Rep 2021;10:32-41. [Crossref] [PubMed]
- de Leeuwerk ME, Bor P, van der Ploeg HP, et al. The effectiveness of physical activity interventions using activity trackers during or after inpatient care: a systematic review and meta-analysis of randomized controlled trials. Int J Behav Nutr Phys Act 2022;19:59. [Crossref] [PubMed]
Cite this article as: Cotton JL, Abbitt D, Carmichael H, Iguidbashian J, Suarez-Pierre A, Meguid RA, Rove JY, Jones EL, Jones TS, Robinson TN. Returning to baseline daily ambulation after cardiothoracic surgery. Video-assist Thorac Surg 2022;7:23.