
Non-intubated video-assisted pulmonary metastasectomy: a narrative literature review
Introduction
Lungs are the second most frequent metastatic site following the liver. Nearly 30% of patients affected by a solid malignant tumor, will further develop pulmonary metastasis (1,2). Surgical resection of lung metastases is considered a valid therapeutic option for different malignant diseases. Pulmonary metastasectomy (PM) is generally indicated in patients who can tolerate single or multiple resections and when all lesions can be radically removed (3).
To date, there are no clear guidelines on the optimal surgical approach and type of resection for this group of patients; the role of lymph node assessment is not clearly defined as well. Nevertheless, there is unanimous consent, among thoracic surgeons, that the primary endpoint of PM should be to achieve radical resection of all suspected metastatic lesions while sparing as much lung parenchyma as possible.
The open surgical approach has been considered, in the past, as the preferred approach to lung metastasectomy, as it allows bimanual palpation of the parenchyma avoiding missing undetected small lesions not displayed by preoperative chest CT scan (4).
Driven by success in the treating of primary lung malignancies the video-assisted thoracoscopic surgery (VATS) gradually carved out a role even for PM, claiming its clinical and technical advantages especially for isolated pulmonary nodules resection (5,6).
The evolution of non-intubated thoracic surgery (NITS) techniques has pushed surgeons to progressively adopt the non-intubated approach to perform more complicated operations in patients with different lung diseases (7). NITS proved to be easily accepted and well tolerated by patients with low morbidity, faster postoperative recovery, and similar long-term oncological results, compared to those undergoing standard general anesthesia (8).
We present the following article in accordance with the Narrative Review reporting checklist (available at https://dx.doi.org/10.21037/vats-21-30).
Methods
We conducted a literature search on PubMed databases through January 31st, 2021, with the following keywords: “pulmonary metastasectomy”, “lung metastasectomy”, “Video-assisted Thoracic Surgery”, “VATS”, “awake surgery”, “non-intubated surgery”.
We retrieved articles concerning the management of lung metastasis with a minimally invasive approach and the use of non-intubated technique, aiming to clarify its current role and indications.
The references of all analyzed articles were screened for relevant papers not found in the initial search. Finally, the information from the studies with the best contributions was synthesized to a narrative form.
Discussion
Oncological background
Historically, the first published report of PM dates back to 1882 when the resection of two incidental pulmonary nodules was performed during the surgical excision of a chest wall sarcoma (9). More than half a century later, in 1947, Alexander and Haight reported the earliest series of resection of solitary pulmonary metastases in 24 patients and the results of a 3-year follow-up (10).
In 1997, Pastorino et al. published the results of the International Registry of Lung Metastases, reporting on 5,206 PM with a 5-year overall survival (OS) of 13% to 36%, depending on primary tumor histology; the authors concluded that surgical resection of lung metastases is a safe and potentially curative procedure (11).
Since then, a large number of published studies have supported the safeness and oncologic benefits of lung metastasectomy.
Primary tumor biology remains the principal prognostic indicator in the management of metastatic disease. To date, current literature reports 5- and 10-year survival rates of 20% to 48% and 15.8% to 37.7%, respectively, for all primary cancers following lung metastasectomy. Among different primary tumor histology, germ cell tumor metastases showed a positive 5- and 10-year survival, ranging between 42% to 82% and 63% to 86%, respectively (12).
The disease-free interval (DFI), defined as the time between the treatment of primary tumor and the diagnosis of lung metastases is directly associated with survival. The majority of the studies agreed that a DFI of less than 36 months is correlated with poor survival (13).
Radical resection is considered the main goal of surgical treatment and has proved to be the most important predictor of survival following PM (14,15).
Eligibility criteria for surgical metastasectomy are summarized in Table 1 (13,16-18).

Full table
VATS metastasectomy
Traditionally, bimanual palpation, during lung metastasectomy, has been considered the most appropriate approach to achieve complete resection of all metastatic lesions, including small nodules not identified on preoperative imaging (19,20). Unilateral metastases were usually approached via thoracotomy, while sternotomy, clamshell thoracotomy, or sequential bilateral thoracotomies were the preferred approaches to manage bilateral metastatic lesions. Nevertheless, with the widespread of VATS for the treatment of numerous primary lung diseases, thoracic surgeons have challenged the need for open approaches to lung metastasectomy. VATS has shown several potential advantages over traditional open thoracotomy. VATS has been proved to cause less immunological impairment after surgery compared to thoracotomy; in particular, it results in a lower production of proinflammatory cytokines and in a lower reduction of natural killer cells, which are well known to be implicated in tumor immunosurveillance (21,22). The impact of this immunologic effect on cancer patients is still unproven; however, theoretically, benefits may be relevant in patients with metastatic diseases with increasing evidence for immune escape mechanisms in cancer metastasis (23,24). In 2015, the CALGB (Cancer and Leukemia Group B) study, have demonstrated that VATS lobectomy is associated with shorter in-hospital stay and less postoperative complications compared with the open approach (25). Quick recovery and minimized systemic insult are paramount in patients with metastatic disease, as surgery will often be followed with systemic therapy; delays resulted from prolonged hospitalization and deconditioning should be avoided. To date, there is no randomized comparison of the minimally invasive thoracoscopic approach to traditional open techniques for the management of metastatic diseases to the lungs. However, several authors have recently reported their experiences with VATS versus open lung metastasectomy. The historical issue on the concept of “missed lesions” during VATS metastasectomy has been the focus of numerous studies. Cerfolio and colleagues published a retrospective analysis of 57 patients who underwent thoracotomy for metastatic pulmonary disease; all patients were retrospectively considered eligible for VATS resection. In 21 out of 57 patients, bimanual palpation identified nodules that were not detected by preoperative chest CT scan. Nevertheless, in only 10 of these 21 patients, the CT scan missed nodules resulted as metastatic lesions on final pathological evaluation. The authors concluded that bimanual palpation led to the resection of benign nodules in 19.3% of patients (26). More recently in 2014, Eckardt et al. published the results of a prospective study of open versus thoracoscopic approach for PM. The investigators observed that only 87% of the lesions detected on preoperative CT scans were identified during the VATS procedures. On the contrary, in the thoracotomy group, additional 67 nodules were identified, of which 22 (33%) resulted as metastatic lesions (27). These studies show that bimanual palpation, compared to VATS, may identify small lesions that are even undetected by CT scanning; however, the effect of the missed nodules on the oncologic outcome (in terms of overall or disease-specific survival) remains undetermined.
A proposed explanation is that these “missed” lesions can remain dormant or develop throughout the tumor history, representing the natural biology of cancers that grow at different speed rates and may explain the fact that post-resection recurrence rate is frequently over 50% even after thoracotomy (11). The complete resection of all palpable metastatic nodules by open surgery does not always determine that complete resection of the metastatic disease is achieved, and, interestingly, multiple subsequent resections of lung metachronous metastases do not significantly affect the OS (28).
Nakajima et al., published in 2008, a retrospective study comparing 72 patients who underwent VATS, with 71 patients who received thoracotomy for colorectal lung metastases. They observed that the 5-year recurrence-free survival was improved in the VATS group (34.4% vs. 21.1%, P=0.047) with no difference in OS (49.3% vs. 39.5%) (29). Supportive results were also reported by Gossot and colleagues, in 2009. The authors compared patients undergoing wedge resections by VATS (31 patients) and thoracotomy (29 patients), for the treatment of sarcoma lung metastases. Patients included in this study had two or more lung lesions that were no larger than 3 cm. The analysis found similar OS (P=0.2) and disease-free survival (P=0.74) between the VATS and thoracotomy groups. However, a significant reduction in the postoperative stay was observed in the VAST group (3.7 vs. 6.2 days; P<0.0001). The results of this study suggested that the shorter hospital stay and the preserved ability to undergo repeated metastasectomy could be potential benefits of the thoracoscopic approach (30).
Abdelnour-Berchtold et al. analyzed a consecutive series of 77 patients undergoing VATS metastasectomy for ≤3 peripheral lesions and noted that the procedure was well tolerated and allowed for a complete resection in all patients, with an OS of 54% at 5 years and a recurrence rate of 30%. The authors concluded that setting those criteria, VATS metastasectomy seems to be associated with a similar outcome compared to the conventional thoracotomy approach concerning survival and local recurrence while reducing postoperative morbidity, especially in situations where a redo procedure is needed (31).
The importance of VATS should also be mentioned for its role in diagnosis. Pulmonary nodules detected during oncological follow-up in patients with known malignancies may be difficult to differentiate from primary lung tumors; thoracoscopic resection is the preferred diagnostic approach and offers a therapeutic benefit in patients with fewer than three lesions (28,31). Bellier and colleagues found that 50% of pulmonary nodules in patients with known malignancy were metastases whereas 26% were newly primary lung cancers. The lack of radiologic parameters to discriminate them endorsed the necessity of histological assessment to avoid diagnostic uncertainty and suboptimal treatments (32).
Although no prospective trials are currently available, most of the studies reported in the literature support the role of thoracoscopic surgery for the management of lung metastases, in appropriately selected patients and specific situations. The use of minimal invasive VATS approach appears to reduce immunologic insult, morbidity, postoperative complications, and hospital stay compared with standard thoracotomy, providing better acceptance, patient’s quick surgical recovery and preservation of good quality of life, avoiding potential delay in adjuvant therapy, with at least equivalent oncological results (28). With advances in preoperative imaging, only very small lesions (<2 mm) can potentially be missed during thoracoscopic metastasectomy (6). Moreover, pulmonary metastases can recur in the lungs in more than 53% of metastatic patients; repeat thoracoscopic lung metastasectomy appears to be a reasonable strategy for the treatment of recurrent lesions (11).
Non-intubated VATS (NI-VATS) metastasectomy
Lung surgery with tracheal intubation and “one-lung” ventilation has proved to be related to several adverse effects in systemic inflammation and immunology response (33). Inflammatory markers and immune phenotype are promising prognostic indicators to differentiate subsets of patients who could benefit best from PM (34). Unfortunately, some patients operated for lung metastases develop unexpected new lung lesions after short-term follow-up. The immune-depressive effect and the biological perturbations that accompany the surgical stress response, which are greater in open surgery vs. VATS and in tracheal intubation vs. non-intubation was reported to be associated with shorter DFIs and time-to-recurrence and paradoxically might also promote disease recurrence or the progression of metastatic disease (35,36).
In the last decade, several authors have investigated the potential positive effects of non-intubated anesthesia on inflammatory stress response; the non-intubated operations showed to be associated with a lesser degree of immunologic depression and lower level of inflammation compared to traditional intubated surgery (37,38).
The favorable impact of NITS on immunologic response appears to be particularly suitable for the surgical treatment of oligometastatic patients.
Patients’ sedation together with loco-regional anesthesia, such as thoracic epidural anesthesia (TEA), allows VATS to be performed safely, avoiding adverse effects of general anesthesia, selective ventilation, and minimizing the negative side effects of tracheal intubation. TEA, in particular, has been demonstrated to decrease cardiac morbidity and mortality after non-cardiac surgery, reduction of pulmonary complications due to earlier mobilization, reduced opioid consumption, and adequate pain relief for coughing (39). Furthermore, patients may benefit from the efficient contraction of the dependent hemidiaphragm and preserved hypoxic pulmonary vasoconstriction during surgically induced pneumothorax in spontaneous ventilation (40,41).
The feasibility and clinical outcome of NITS have been investigated in two recent meta-analyses by Bertolaccini et al. in 2017 and Zhang and colleagues in 2019. The authors reported the results of awake, NI-VATS procedures for different lung diseases (such as bullectomies, wedge resections, lobectomies, lung volume reduction operations, sympathectomies, and talc pleurodeses) performed in a heterogeneous group of patients. NIST showed a significantly lower postoperative complication rate, length of stay, and shorter duration of anesthesia compared to the control group of traditionally intubated surgery. The favorable results of the initial experience with NITS suggest extending indications to a non-intubated approach even for surgical procedures in patients with high comorbidity indexes, reduced cardiovascular function, and functional conditions contraindicating general anesthesia (42,43).
In 2017, Mineo et al. presented the short- and long-term results of 71 patients, with pulmonary metastases, who underwent VATS metastasectomy under non-intubated anesthesia. There was no reported mortality and major comorbidity was described in four out 71 patients (5.5%). Median hospital stays were 3 (range, 2–4) days, and the chest tube was removed after a median time of 14 (range, 10–31) hours. Post-operative disease-free and OS at 3 years were 17% and 49%, respectively, similar to those achieved with intubated surgery. The authors concluded that VATS metastasectomy combined with non-intubated anesthesia can be safely performed in patients with lung oligometastases, with long-term results comparable to traditional open surgery. They reported, also, significant advantages in the overall operative time and length of in-hospital stay, thus meeting better patient satisfaction and lower economical costs (44).
Indications to NI-VATS metastasectomy are still not widely codified, however, patients could be considered eligible to undergo this procedure if they meet specific requirements. First of all, patients should meet the classic prerequisite for PM, as mentioned above and summarized in Table 1. Secondary, all candidates suitable for VATS resection of a pulmonary nodule are theoretically eligible for an awake approach: imaging negative for the presence of pleural adhesion, mass body index lower than 30 kg/m2, and absence of bleeding disorders. Lung metastasis should be located in a peripheral position, with the large diameter smaller than 3 cm, easy to be detected with single-finger or instrumental inspection, and/or amenable to be resected with wedge resection or through precision resection with electrocautery (7).
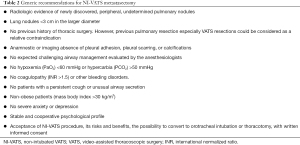
Concerning the specific criteria for NITS, many authors agreed that this newly developed surgical modality requires extra attention to some particular aspects: surgeon must have knowledge of this method and extensive experience in VATS technique; anesthesiologist should have assessed the easy accessibility to the airways and/or risk factors resulting in adverse tracheobronchial conditions; and patients should have a stable and cooperative psychological profile (44,45). Paradoxically, the recommendations for NI-VATS have been established in patients with increased risk for general anesthesia, thus high-risk patients with pre-existing pulmonary disease and elderly patients should be the categories who benefit more from awake surgery (46).
Current recommendations for NI-VATS metastasectomy are listed in Table 2 (7,41,44-46).
Full table
Summary
VATS metastasectomy is gaining growing interest among general thoracic surgeons as a curative procedure, challenging the traditional dogma of the need for bimanual lung palpation through an open approach. Several studies reported that there is no difference between the open and VATS approaches in terms of local control and long-term survival.
The role of VATS lung metastasectomy under non-intubated anesthesia is still under investigation, though. NITS seems to offer a valid alternative to the conventional VATS approach, enhancing its benefits particularly re-including the surgical treatment in the management of metastatic disease of patients with high risk for general anesthesia.
However, it is also true that, to date, very few studies reporting on the initial results of this procedure are available. These studies are mostly single-center trials enrolling a small number of patients.
Larger randomized prospective (possibly multicentric) studies are advocated to outline the role, specific indications, and long-term benefits of NIST procedures in metastatic patients.
Acknowledgments
Funding: None
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Francesco Guerrera, Paolo Albino Ferrari and Roberto Crisci) for the series “Non-Intubated Thoracic Surgery. A Global Perspective” published in Video-Assisted Thoracic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://dx.doi.org/10.21037/vats-21-30
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/vats-21-30). The series “Non-Intubated Thoracic Surgery. A Global Perspective” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Downey RJ. Surgical treatment of pulmonary metastases. Surg Oncol Clin N Am 1999;8:341. [Crossref] [PubMed]
- Quiros RM, Scott WJ. Surgical treatment of metastatic disease to the lung. Semin Oncol 2008;35:134-46. [Crossref] [PubMed]
- Rusch VW. Pulmonary metastasectomy. Current indications. Chest 1995;107:322S-31S. [Crossref] [PubMed]
- Downey RJ, Bains MS. Open surgical approaches for pulmonary metastasectomy. Thorac Surg Clin 2016;26:13-8. [Crossref] [PubMed]
- Sonett JR. Pulmonary metastases: biologic and historical justification for VATS. Video assisted thoracic surgery. Eur J Cardiothorac Surg 1999;16:S13-5; discussion S15-6. [Crossref] [PubMed]
- Servais E, Swanson SJ. Thoracoscopic management of pulmonary metastases. Thorac Surg Clin 2016;26:91-7. [Crossref] [PubMed]
- Pompeo E, Mineo TC. Awake operative videothoracoscopic pulmonary resections. Thorac Surg Clin 2008;18:311-20. [Crossref] [PubMed]
- Pompeo E, Mineo TC. Awake pulmonary metastasectomy. J Thorac Cardiovasc Surg 2007;133:960-6. [Crossref] [PubMed]
- Weinlechner J. Tumoren an der brustwand und deren behnadlung resection der rippeneroffnung der brusthohle und partielle entfernung der lunge. Wien Med Wochenschr 1882;32:589-91.
- Alexander J, Haight C. Pulmonary resection for solitary metastatic sarcomas and carcinomas. Surg Gynecol Obstet 1947;85:129-46. [PubMed]
- Pastorino U, Buyse M, Friedel G, et al. Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. J Thorac Cardiovasc Surg 1997;113:37-49. [Crossref] [PubMed]
- Cheung FP, Alam NZ, Wright GM. The past, present and future of pulmonary metastasectomy: a review article. Ann Thorac Cardiovasc Surg 2019;25:129-41. [Crossref] [PubMed]
- Pastorino U. Lung metastasectomy: why, when, how. Crit Rev Oncol Hematol 1997;26:137-45. [Crossref] [PubMed]
- Younes RN, Abrao F, Gross J. Pulmonary metastasectomy for colorectal cancer: long-term survival and prognostic factors. Int J Surg 2013;11:244-8. [Crossref] [PubMed]
- Murthy SC, Kim K, Rice TW, et al. Can we predict long-term survival after pulmonary metastasectomy for renal cell carcinoma? Ann Thorac Surg 2005;79:996-1003. [Crossref] [PubMed]
- Sudarshan M, Murthy SC. Current indications for pulmonary metastasectomy. Surg Oncol Clin N Am 2020;29:673-83. [Crossref] [PubMed]
- Kondo H, Okumura T, Ohde Y, et al. Surgical treatment for metastatic malignancies. Pulmonary metastasis: indications and outcomes. Int J Clin Oncol 2005;10:81-5. [Crossref] [PubMed]
- Erhunmwunsee L, D'Amico TA. Surgical management of pulmonary metastases. Ann Thorac Surg 2009;88:2052-60. [Crossref] [PubMed]
- Margaritora S, Porziella V, D'Andrilli A, et al. Pulmonary metastases: can accurate radiological evaluation avoid thoracotomic approach? Eur J Cardiothorac Surg 2002;21:1111-4. [Crossref] [PubMed]
- McCormack PM, Bains MS, Begg CB, et al. Role of video-assisted thoracic surgery in the treatment of pulmonary metastases: results of a prospective trial. Ann Thorac Surg 1996;62:213-6; discussion 216-7. [Crossref] [PubMed]
- Ng CS, Wan S, Hui CW, et al. Video-assisted thoracic surgery for early stage lung cancer - can short-term immunological advantages improve long-term survival? Ann Thorac Cardiovasc Surg 2006;12:308-12. [PubMed]
- Yim AP, Wan S, Lee TW, et al. VATS lobectomy reduces cytokine responses compared with conventional surgery. Ann Thorac Surg 2000;70:243-7. [Crossref] [PubMed]
- Croci DO, Salatino M. Tumor immune escape mechanisms that operate during metastasis. Curr Pharm Biotechnol 2011;12:1923-36. [Crossref] [PubMed]
- Pancione M, Giordano G, Remo A, et al. Immune escape mechanisms in colorectal cancer pathogenesis and liver metastasis. J Immunol Res 2014;2014:686879 [Crossref] [PubMed]
- Nwogu CE, D'Cunha J, Pang H, et al. VATS lobectomy has better perioperative outcomes than open lobectomy: CALGB 31001, an ancillary analysis of CALGB 140202 (Alliance). Ann Thorac Surg 2015;99:399-405. [Crossref] [PubMed]
- Cerfolio RJ, McCarty T, Bryant AS. Non-imaged pulmonary nodules discovered during thoracotomy for metastasectomy by lung palpation. Eur J Cardiothorac Surg 2009;35:786-91; discussion 791. [Crossref] [PubMed]
- Eckardt J, Licht PB. Thoracoscopic or open surgery for pulmonary metastasectomy: an observer blinded study. Ann Thorac Surg 2014;98:466-9; discussion 469-70. [Crossref] [PubMed]
- Perentes JY, Krueger T, Lovis A, et al. Thoracoscopic resection of pulmonary metastasis: current practice and results. Crit Rev Oncol Hematol 2015;95:105-13. [Crossref] [PubMed]
- Nakajima J, Murakawa T, Fukami T, et al. Is thoracoscopic surgery justified to treat pulmonary metastasis from colorectal cancer? Interact Cardiovasc Thorac Surg 2008;7:212-6; discussion 216-7. [Crossref] [PubMed]
- Gossot D, Radu C, Girard P, et al. Resection of pulmonary metastases from sarcoma: can some patients benefit from a less invasive approach? Ann Thorac Surg 2009;87:238-43. [Crossref] [PubMed]
- Abdelnour-Berchtold E, Perentes JY, Ris HB, et al. Survival and Local Recurrence After Video-Assisted Thoracoscopic Lung Metastasectomy. World J Surg 2016;40:373-9. [Crossref] [PubMed]
- Bellier J, Perentes JY, Abdelnour-Berchtold E, et al. A plea for thoracoscopic resection of solitary pulmonary nodule in cancer patients. Surg Endosc 2017;31:4705-10. [Crossref] [PubMed]
- Gothard J. Lung injury after thoracic surgery and one-lung ventilation. Curr Opin Anaesthesiol 2006;19:5-10. [Crossref] [PubMed]
- Ghanim B, Schweiger T, Jedamzik J, et al. Elevated inflammatory parameters and inflammation scores are associated with poor prognosis in patients undergoing pulmonary metastasectomy for colorectal cancer. Interact Cardiovasc Thorac Surg 2015;21:616-23. [Crossref] [PubMed]
- Tang F, Tie Y, Tu C, et al. Surgical trauma-induced immunosuppression in cancer: Recent advances and the potential therapies. Clin Transl Med 2020;10:199-223. [Crossref] [PubMed]
- Hiller JG, Perry NJ, Poulogiannis G, et al. Perioperative events influence cancer recurrence risk after surgery. Nat Rev Clin Oncol 2018;15:205-18. [Crossref] [PubMed]
- Koltun WA, Bloomer MM, Tilberg AF, et al. Awake epidural anesthesia is associated with improved natural killer cell cytotoxicity and a reduced stress response. Am J Surg 1996;171:68-72; discussion 72-3. [Crossref] [PubMed]
- Koltun WA, McKenna KJ, Rung G. Awake epidural anesthesia is effective and safe in the high-risk colectomy patient. Dis Colon Rectum 1994;37:1236-41. [Crossref] [PubMed]
- Kao MC, Lan CH, Huang CJ. Anesthesia for awake video-assisted thoracic surgery. Acta Anaesthesiol Taiwan 2012;50:126-30. [Crossref] [PubMed]
- Pompeo E, Sorge R, Akopov A, et al. Non-intubated thoracic surgery-A survey from the European Society of Thoracic Surgeons. Ann Transl Med 2015;3:37. [PubMed]
- Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. [Crossref] [PubMed]
- Bertolaccini L, Zaccagna G, Divisi D, et al. Awake non-intubated thoracic surgery: an attempt of systematic review and meta-analysis. Video-assist Thorac Surg 2017;2:59. [Crossref]
- Zhang K, Chen HG, Wu WB, et al. Non-intubated video-assisted thoracoscopic surgery vs. intubated video-assisted thoracoscopic surgery for thoracic disease: a systematic review and meta-analysis of 1,684 cases. J Thorac Dis 2019;11:3556-68. [Crossref] [PubMed]
- Mineo TC, Sellitri F, Fabbi E, et al. Uniportal non-intubated lung metastasectomy. J Vis Surg 2017;3:118. [Crossref] [PubMed]
- AlGhamdi ZM, Lynhiavu L, Moon YK, et al. Comparison of non-intubated versus intubated video-assisted thoracoscopic lobectomy for lung cancer. J Thorac Dis 2018;10:4236-43. [Crossref] [PubMed]
- Passera E, Rocco G. Awake video-assisted thoracic surgery resection of lung nodules. Video-assist Thorac Surg 2018;3:3. [Crossref]
Cite this article as: Gherzi L, Ferrari M, Pardolesi A. Non-intubated video-assisted pulmonary metastasectomy: a narrative literature review. Video-assist Thorac Surg 2021;6:27.


