The tips of rt. S6 segmentectomy in uniportal VATS segmentectomy
Uniportal video-assisted thoracoscopic surgery (VATS) seems to have acquired more proponents and doers lately as it was the case with the single-port laparoscopic surgery since its promotion, despite the fact that single-port thoracoscopic surgery is the younger method compared to single-port gynecological surgery (1992) and single-port laparoscopic surgery (1999) (1,2).
Thoracic surgeons all over the world seem to believe increasingly that this method really contains enough benefits compared to the traditional thoracoscopic approach, so that it is worth learning. Although supported by the numerous studies, mostly observational without a true comparison between the two modalities—thus of a lower level of evidence, and only one randomized controlled trial being an exception showing no short term benefit (3), it seems like they are enough for now—the technique is still new and no long-term results are to be expected yet.
Assuming that this approach has at least no disadvantages compared to the traditional three-port technique, it should automatically be better, having only one incision, hence less trauma (speculative), less incisional pain and better cosmetics (never confirmed, besides very subjective).
It seems however to be prestigious, being able to perform a uniportal VATS resection. Uniportal VATS is—without a doubt—a more demanding surgical approach that more than a few experienced surgeons gave up trying to learn (personal communication), thinking there might be a risk for their reputation to attend a course or a workshop together with the younger colleagues. Some others invited the most prominent proponents of this approach to serve as a proctor, expecting it to shorten their learning curve. So it is a big question mark now if this technique is in fact an approach applicable by younger surgeons only.
While lobectomies are the gold standard and seem to eventually be manageable by means of uniportal VATS even by beginners, segmentectomies are the real challenge, even for the experienced; they are demanding even by means of traditional VATS too.
The way I perform uniportal VATS apical segmentectomies of the lower lobes is different than that how the majority does them. Early in my practice I realized the benefits of adaptability, so instead of making an incision in front of the lung, at fourth or fifth intercostal space at the mid-axillary line, I decided to make it through the sixth intercostal space, at the back of the lung, in the triangle of auscultation, where the muscle layer was the thinnest and so was the fat tissue. The perspective changed, while the camera was approaching from behind.
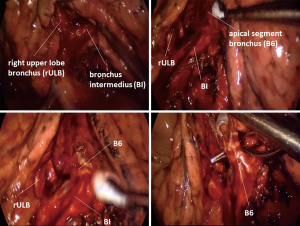
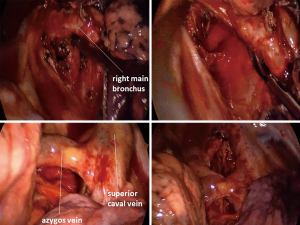
In posterior uniportal VATS on the right side, the dissection begins at the posterior hilum. Pulmonary ligament may be dissected; it is not a necessity though. The goal is to expose the bronchial tree, the upper lobe carina more precisely. It is easily done by following the right main bronchus caudally (Figure 1).
A thoracoscope used in most of the resections was 10 mm 45º, although 30º as well as 5 mm thoracoscope (in both form) have been used. The problem with the 5 mm thoracoscope was relatively insufficient lighting, which is certainly something that shall remain the remnant of the past. Modern thoracoscope do not have this problem anymore, which is why 5mm thoracoscope should have clear priority.
As soon as the mediastinal pleura is divided at posterior hilum, one can bluntly dissect towards the upper lobe carina, where mostly a lymph node exists. It is known that behind and a bit above the node lies the pulmonary artery.
From that point, there are two options for me. The first option is to dissect carefully towards the pulmonary artery exposing its upper edge. At this location it is not very complicated to make a tunnel between the pulmonary parenchyma above (fissural tissue) and the pulmonary artery below, followed by the placement of a stapler in the tunnel to divide it completely (notice: there is no dissection in the fissure). This option is convenient for both right and left lungs, yet to my experience more often applied on the left side (4).
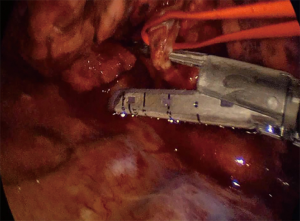
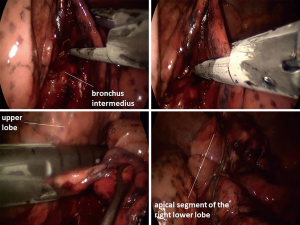
The second option would be to follow the bronchus intermedius caudally for a few centimeters, where S6 bronchus arises. Here one can dissect bluntly around it and even encircle the bronchus. The encircling of the bronchus needs to be careful, as the S6 artery lies very close to the bronchus. However, a good view and an appropriate instrumentation make this undertaking not very complicated. Once the bronchus is encircled a 30-mm stapler is used to divide it. Placing the stapler can easily be done in most cases. If it is challenging, a 20Ch silicone (Robinson) drain (my personal preference) or a Foley catheter can be passed around the bronchus, pulled out of the incision and fed with the thinner anvil of the stapler, then pulled into the pleural cavity to place the stapler in position around the bronchus easily. Alternatively a curved-tip stapler can be used as well (Figure 2).
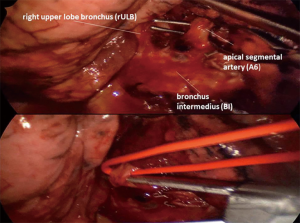
If you decide to go with the fissure-first method, you will be having a partially opened fissure and easily detectable pulmonary artery and its branches; posterior ascending artery (maybe A2 on the left as well) and A6. Before you go for them it may be smart to remove the lymph node lying between them and the bronchial tree (station 11). Following the removal of the node, you can go for the artery without much trouble, either with hemoclips, sutures, some surgical energy device or preferably a stapler. In some cases it can be better to encircle the bronchus first, especially if you will divide A6 with a stapler (Figure 3).
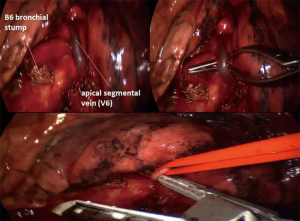
In some cases, V6 is perfectly visible at the hilum, right at the beginning of the dissection. You may choose to go for it, or to save it for the end. In most cases this vein becomes visible only after the division of both A6 and B6, and sometimes even after the fissure is divided and S6 is pulled up and away from the bronchial tree. It crosses the bronchus intermedius caudally; actually at this point it is more difficult not to see it (Figure 4).
Inflation of the lung is the most useful method for distinguishing the borders of the S6 from the adjacent segments. It is very valuable, yet sometimes it can be useless as the lung becomes completely inflated. In that case, the next deflation can be helpful, due to the faster removal (washing out) of the air from the unclamped segments of the lung, while S6 needs time to collapse. Bronchoscopy is another useful method, but only to verify if everything is as expected. Following the bronchial division step, the resection can go on with multiple staples of the parenchyma (5) (Figure 5, Video 1).
Lymph node dissection is a crucial part of an anatomical lung resection, if the diagnosis is a lung cancer. It is very convenient to perform it from the posterior approach, dissecting directly in front of the camera. Dissecting at stations 2,4 (and 5,6 on the left side) can be time consuming, yet a complete dissection, is warranted. Left side is a bit more challenging and the question is how much and how deep one would want to dig in aorto-pulmonary window (not to endanger the recurrent nerve). To my opinion this dilemma remains regardless of the approach (Figure 6, Video 2).
In case of a necessity to proceed with lobectomy, the incision fulfill its purpose nevertheless (6).
In conclusion, S6 resection is very straight forward with posterior uniportal VATS technique. Anatomical variations are possible, yet not very often and certainly hard to miss with this approach. The incision of the posterior approach is smaller and the entrance more narrow, yet with the proper positioning on the table it is completely sufficient. The chest tube is going to be on the back of the patient but this does not seem to be increasing the pain or discomfort so far (6,7) (Figure 7).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Hitoshi Igai) for the series “Uniportal VATS Segmentectomy” published in Video-Assisted Thoracic Surgery. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2019.12.03). The series “Uniportal VATS Segmentectomy” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kirshtein B, Haas EM. Single port laparoscopic surgery: concept and controversies of new technique. Minim Invasive Surg 2012;2012:456541 [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Perna V, Carvajal AF, Torrecilla JA, et al. Uniportal video-assisted thoracoscopic lobectomy versus other video-assisted thoracoscopic lobectomy techniques: a randomized study. Eur J Cardiothorac Surg 2016;50:411-5. [Crossref] [PubMed]
- Stamenovic D. Uniportal Posterior Approach for Videothoracoscopic Anatomical Resection of Apical Segment of the Left Lower Lobe. CTSNet. 2016; Published 16 May 2016, accessed 18.01.2017. Available online: https://www.ctsnet.org/article/uniportal-posterior-approach-videothoracoscopic-anatomical-resection-apical-segment-left
- Stamenovic D. Uniportal Posterior Approach for Videothoracoscopic Anatomical Resection of Posterior Segment of the Right Upper Lobe. CTSNet. 2017; Published 04 January 2017, accessed 18 January 2017. Available online: https://www.ctsnet.org/article/uniportal-posterior-approach-videothoracoscopic-anatomical-resection-posterior-segment-right
- Stamenovic D, Bostanci K, Messerschmidt A. Posterior uniportal video-assisted thoracoscopic surgery for anatomical lung resections. J Thorac Dis 2017;9:5261-6. [Crossref] [PubMed]
- Stamenovic D, Messerschmidt A. Posterior uniportal video-assisted thoracoscopic surgery for resection of the apical segment of the right lower lobe followed by completion lobectomy. Interact Cardiovasc Thorac Surg 2017;24:644-5. [PubMed]
Cite this article as: Stamenovic D. The tips of rt. S6 segmentectomy in uniportal VATS segmentectomy. Video-assist Thorac Surg 2020;5:16.