
Modified tube fixation technique for uniportal video-assisted thoracic surgery
Introduction
As the development of video-assisted thoracoscopic surgery (VATS), uniportal VATS has gained more and more attention for its obvious benefits compared with conventional multi-port VATS, such as less postoperative pain, fewer paresthesias, higher patient satisfaction (1-4) and the direct view to the target tissue (5). With the uniportal VATS, the surgery could be done like open operations (6,7), which are familiar to surgeons. Conventionally, a chest tube drain is placed through the port incision site or a new incision site on another intercostal space 1 level downward and secured to the skin by tacking sutures. However, as we know, there are some shortcomings in this conventional tube fixation, such as leakage of fluid or air, intra-operative paresthesia and post-operative in aesthetic scar caused by the anchoring suture, which may lower the patients’ satisfaction. To overcome these shortcomings, we designed a new tube fixation technique for uniportal VATS.
Technique
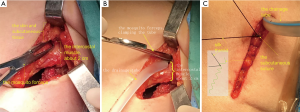
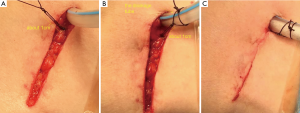
The details are as follows (Figures 1,2). First, when the uniportal VATS was completed, the skin and subcutaneous tissue were pulled up and the intercostal muscle in the same intercostal space was transpierced with a mosquito forceps about 2.0 cm beyond the distal end of the incision site. Second, the drainage tube was clamped and punctured into the cavity, which is as alike as the procedure of doing a chest drainage that is familiar to thoracic surgeons in general. Third, after the drainage tube was placed properly, the subcutaneous tissue was sutured conventionally. Fourth, the drainage tube was anchored about 1.0 cm beyond the incision with a silk thread which was passed through the subcutaneous suture. Finally, the skin incision was closed by subcutaneous continuous suture with a 3-0 self-retaining suture (Quill TM knotless tissue-closure device, Angiotech Puerto Rico Inc., Vancouver, Canada) which was cut flush to the skin lastly. When remove, one end of the anchoring silk thread was snipped and the drainage tube was pulled out which just like removing the stiches, and the wound was sealed with Vaseline gauze immediately.
Comment
As the development of VATS and enhanced recovery after surgery (ERAS), more attention has been paid to reduce post-operative pain and improve the aesthetic outcomes. And, many efforts have been made. Son et al. (2) reported a modified incision and closure technique for uniportal VATS. In their technique the skin is incised lower than an intercostal muscle incision, and the chest tube transpierces the chest wall muscle about 1 cm below the incision. Finally, nylon is used for tube fixation and is anchored through the subcutaneous suture. It was valid, and applied about 20 cases in our department. However, we found that was somewhat intricate especially at the first few cases. Moreover, there was more trauma in their technique because more dissection between the subcutaneous tissue and chest wall muscle was performed. It did not meet the standard of mini-invasiveness. Furthermore, it increased the difficulty and time of conversion to an open surgery if needed in their technique.
To conclude, our new tube fixation technique for SITS is effective with less trauma and a better cosmetic effect, and easy to perform.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2018.10.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [Crossref] [PubMed]
- Son BS, Park JM, Seok JP, et al. Modified incision and closure techniques for single-incision thoracoscopic lobectomy. Ann Thorac Surg 2015;99:349-51. [Crossref] [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [Crossref] [PubMed]
- Mier JM, Chavarin A, Izquierdo-Vidal C, et al. A prospective study comparing three-port video-assisted thoracoscopy with the single-incision laparoscopic surgery (SILS) port and instruments for the video thoracoscopic approach: a pilot study. Surg Endosc 2013;27:2557-60. [Crossref] [PubMed]
- Hsu PK, Lin WC, Chang YC, et al. Multiinstitutional analysis of single-port video-assisted thoracoscopic anatomical resection for primary lung cancer. Ann Thorac Surg 2015;99:1739-44. [Crossref] [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5:S214-6. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5:S234-45. [PubMed]
Cite this article as: Du X, Chen G, Tian D, Xie L, Zhou H. Modified tube fixation technique for uniportal video-assisted thoracic surgery. Video-assist Thorac Surg 2018;3:45.


