
Awake non-intubated thoracic surgery: an attempt of systematic review and meta-analysis
Introduction
The challenge of surgeons in our era is a less-invasive procedure. Over the last 20 years, video assisted thoracic surgery (VATS) become the treatment of choice in multiple chest related illnesses. Usually, VATS requires general anaesthesia with the selective intubation (1,2). However, in severe patients, with a high comorbidity index or elevated risk for anaesthesia, general anaesthesia may not be possible. An alternative is to perform the VATS in patients under local anaesthesia, awake, and non-intubated (3-5). We conducted a systematic literature review and meta-analysis of non-intubated VATS (AVATS) focusing attention on mortality rate, the complications and the hospital length of stay.
Material and methods
We designed a search strategy using a combination of free-text words, relevant MeSH terms and appropriate filters in EMBASE (via Ovid), MEDLINE (via PubMed) and Cochrane CENTRAL from 1997 until 2017, without imposing any language or time restrictions. Records identified by the search strategy were exported into a reference management software. The eligibility criteria were: [(thoracoscopic surgery OR vats) AND (awake OR not intubated OR tubeless OR local anaesthesia) AND outcome]. Two authors assessed each identified study based on the eligibility criteria; when multiple studies contained overlying data, the most informative study was included. We excluded letters, editorials, case reports, and reviews. Disagreements were debated and resolved by consensus. Data extracted included study characteristics, baseline patient characteristics primary and secondary outcomes. The risk of bias of included RCT and has been evaluated following Cochrane recommendations (6). The meta-analysis was attempted by combining the reported survival results of the individual studies using a random effect model. The odds ratio (OR) and standard error were extracted or calculated from each study using Kaplan-Meier graphs with methods reported in the literature (7,8). Confidence intervals (CI) were set to 95%. Heterogeneity was measured using χ2 test and I2. Values of P<0.10 or I2>50% represented substantial heterogeneity. Publication bias was evaluated using the funnel plot. Details of the protocol for this systematic review were registered on PROSPERO (CRD42017072141) and can be accessed at http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017072141. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was used to improve the report of this systematic review (9). Data analysis was performed using Review Manager 5.3 (Nordic Cochrane Centre, Copenhagen, Denmark) (10). For all analyses, P<0.05 was considered statistically significant.
Results
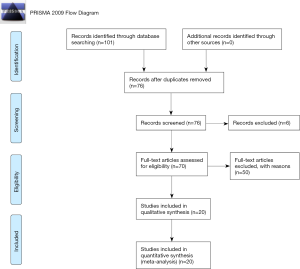
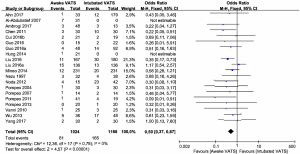
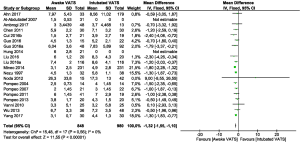
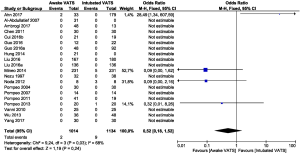
According to PRISMA statement, the flow diagram of the study selection process was showed in Figure 1. The search strategy identified 101 records. Following deduplication, 76 records were screened at the title and abstract level, and six were excluded as irrelevant. The remaining 70 records were assessed in the full text. Of those, 20 were included in the systematic review and meta-analysis (1,11-29). Baseline characteristics of patients were balanced in each study. Most of these qualified studies were based on the retrospective data. The size of the cohorts varied from 14 to 221, with a total number of 1,024 patients. In all calculations, the awake VATS were chosen as the reference. Lack of blinding was not considered likely to influence the primary outcome due to its objective nature. Hence, all studies were at reduced risk of bias despite being open label. It was not possible to demonstrate statistical significance relative to mortality due to the insufficiency of data. Regarding the hospital length of stay, the data suggest that AVATS was characterised by a shorter duration of hospitalisation (Figure 2). The pooled mean difference was −1.32 (95% CI: −1.55 to −1.10; P<0.00001), the Cochrane tests for heterogeneity disclosed that χ2=15.48, degree of freedom =17 (P=0.56); I2=0%. Regarding the complication (Figure 3), the OR was 0.50 (95% CI: 0.37–0.67; P<0.00001), heterogeneity showed that χ2=12.36, degree of freedom =17 (P=0.78) I2=0%. Data demonstrated some benefits of AVATS in patients with high comorbidity index. On the contrary, OR for mortality (Figure 4) showed the absence of statistical significance (OR =0.53; 95% CI: 0.18–1.52; P<0.024).
Discussion
VATS has become a globally accepted alternative to thoracotomy for the surgical treatment of patients with various thoracic conditions involving lung, pleura and mediastinum. Recently, as a less invasive surgical technique, non-intubated VATS under loco-regional anaesthesia has gained increasing widespread attention globally. Excellent outcomes of non-intubated VATS under loco-regional anaesthesia were not only reported in some case reports, but also in some RCT with a small sample size. However, as mentioned above, the currently available studies about non-intubated VATS under loco-regional anaesthesia were all carried out in a small sample size, which lacks robust evidence to elucidate its actual feasibility and safety for thoracic surgery. We conducted an attempt of meta-analysis aiming to establish the safety profile of AVATS. Our data suggested that AVATS exhibited favourable effects in improving the short-term outcomes of patients and yielded significantly shorter in-operating room time and hospital stays, as well as a significantly lower rate of postoperative complications than intubated VATS under general anaesthesia. In patients with incompatibility with general anaesthesia due to significant comorbidity and severe respiratory failure (ASA 4), AVATS was feasible and efficient (3). AVATS is also possible in major lung surgery. Surgical parameters (blood loss, drainage duration, drainage volumes, the length of stay, the rate of complications, etc.) have shown that AVATS is feasible and beneficial compared to VATS in general anaesthesia. In pulmonary resections, the utility of AVATS has also been demonstrated in segmentectomy that is technically possible and how can it be considered a valid alternative in compromised patients. Authors found that AVATS achieved a shorter anaesthesia time which may account for shorter global in-operating room time. In patients treated with AVATS, perioperative mortality was not observed, related to inclusion and exclusion criteria and the reduced invasiveness of AVATS. Therefore, all the evidence proved that AVATS.
Our study presents some limitations. First, the experimental group was very heterogeneous, with epidural, paravertebral, intercostal and other forms of anaesthesia, with and without sedation. Secondly, the surgery performed is highly different from minor procedures in healthy patients to major lung resection to palliation of advanced malignancy. The mortality analyses presented based on these studies (which contain all the events) cannot be used to conclude due to the multiple disease states and operations included.
Conclusions
AVATS is a feasible and safe technique that is increasingly aware of the possibility of applying for surgery even patients with high indexes of comorbidity, reduced cardiovascular function and general conditions contraindicating general anaesthesia. With the reduction in the rate of complications, it allows for shorter stay times, resulting in lower costs for overlapping results or better than VATS in general anaesthesia. With the development of anesthesiology and surgery, an increasing number of patients could benefit from AVATS, and the indications for surgery could be expanded. However, its effects on long-term prognosis need to be verified by establishing prospective, multicentre clinical trials with a large sample size. Nevertheless, further investigations are required to confirm these findings.
Acknowledgments
Funding: None.
Footnote
Provenance and peer review: The article was commissioned by the editorial office, Video-Assisted Thoracic Surgery for the series "VATS Special Issue dedicated to the 4th international VATS Symposium 2017". The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2017.08.17). The series “VATS Special Issue dedicated to the 4th international VATS Symposium 2017” was commissioned by the editorial office without any funding or sponsorship. LB serves as an unpaid editorial board member of Video-Assisted Thoracic Surgery from Jul 2016 to May 2019. RC served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang SM, Wang ML, Hung MH, et al. Tubeless Uniportal Thoracoscopic Wedge Resection for Peripheral Lung Nodules. Ann Thorac Surg 2017;103:462-8. [Crossref] [PubMed]
- Hung MH, Cheng YJ, Hsu HH, et al. Non intubated uniportal thoracoscopic segmentectomy for lung cancer. J Thorac Cardiovasc Surg 2014;148:e234-5. [Crossref] [PubMed]
- Kiss G, Claret A, Desbordes J, et al. Thoracic epidural anaesthesia for awake thoracic surgery in severely dyspnoeic patients excluded from general anaesthesia. Interact Cardiovasc Thorac Surg 2014;19:816-23. [Crossref] [PubMed]
- Liu J, Cui F, Li S, et al. Non intubated video-assisted thoracoscopic surgery under epidural anaesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. [Crossref] [PubMed]
- Hung MH, Hsu HH, Chen KC, et al. Non intubated thoracoscopic anatomical segmentectomy for lung tumors. Ann Thorac Surg 2013;96:1209-15. [Crossref] [PubMed]
- Higgins JP, Green S. editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Updated March 2011. The Cochrane Collaboration, 2011. Available online: http://www.cochrane-handbook.org
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 1998;17:2815-34. [Crossref] [PubMed]
- Guyot P, Ades A, Ouwens MJ, et al. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan–Meier survival curves. BMC Med Res Methodol 2012;12:9. [Crossref] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100 [Crossref] [PubMed]
- Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre TCC, 2014.
- Ahn HY, Kim YD, Cho JS, et al. Thoracoscopic surgery under epidural anesthesia for intractable secondary spontaneous pneumothorax. Asian J Surg 2017;40:285-9. [Crossref] [PubMed]
- Al-Abdullatief M, Wahood A, Al-Shirawi N, et al. Awake anaesthesia for major thoracic surgical procedures: an observational study. Eur J Cardiothorac Surg 2007;32:346-50. [Crossref] [PubMed]
- Ambrogi V, Sellitri F, Perroni G, et al. Uniportal video-assisted thoracic surgery colorectal lung metastasectomy in non-intubated anesthesia. J Thorac Dis 2017;9:254-61. [Crossref] [PubMed]
- Chen JS, Cheng YJ, Hung MH, et al. Non intubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038-43. [Crossref] [PubMed]
- Cui F, Liu J, Li S, et al. Tubeless video-assisted thoracoscopic surgery (VATS) under non-intubated, intravenous anesthesia with spontaneous ventilation and no placement of chest tube postoperatively. J Thorac Dis 2016;8:2226-32. [Crossref] [PubMed]
- Guo Z, Yin W, Zhang X, et al. Primary spontaneous pneumothorax: simultaneous treatment by bilateral non-intubated videothoracoscopy. Interact Cardiovasc Thorac Surg 2016;23:196-201. [Crossref] [PubMed]
- Guo Z, Yin W, Pan H, et al. Video-assisted thoracoscopic surgery segmentectomy by non-intubated or intubated anesthesia: a comparative analysis of short-term outcome. J Thorac Dis 2016;8:359-68. [Crossref] [PubMed]
- Hung MH, Cheng YJ, Chan KC, et al. Non intubated uniportal thoracoscopic surgery for peripheral lung nodules. Ann Thorac Surg. 2014;98:1998-2003. [Crossref] [PubMed]
- Liu J, Cui F, Pompeo E, et al. The impact of non-intubated versus intubated anaesthesia on early outcomes of video-assisted thoracoscopic anatomical resection in non-small-cell lung cancer: a propensity score matching analysis. Eur J Cardiothorac Surg 2016;50:920-5. [Crossref] [PubMed]
- Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. [Crossref] [PubMed]
- Mineo TC, Sellitri F, Tacconi F, et al. Quality of life and outcomes after non intubated versus intubated video-thoracoscopic pleurodesis for malignant pleural effusion: comparison by a case-matched study. J Palliat Med 2014;17:761-8. [Crossref] [PubMed]
- Nezu K, Kushibe K, Tojo T, et al. Thoracoscopic wedge resection of blebs under local anesthesia with sedation for treatment of a spontaneous pneumothorax. Chest 1997;111:230-5. [Crossref] [PubMed]
- Noda M, Okada Y, Maeda S, et al. Is there a benefit of awake thoracoscopic surgery in patients with secondary spontaneous pneumothorax? J Thorac Cardiovasc Surg 2012;143:613-6. [Crossref] [PubMed]
- Pompeo E, Mineo D, Rogliani P, et al. Feasibility and results of awake thoracoscopic resection of solitary pulmonary nodules. Ann Thorac Surg 2004;78:1761-8. [Crossref] [PubMed]
- Pompeo E, Mineo TC. Awake pulmonary metastasectomy. J Thorac Cardiovasc Surg 2007;133:960-6. [Crossref] [PubMed]
- Pompeo E, Tacconi F, Mineo TC. Comparative results of non-resectional lung volume reduction performed by awake or non-awake anesthesia. Eur J Cardiothorac Surg 2011;39:e51-8. [Crossref] [PubMed]
- Pompeo E, Dauri MAwake Thoracic Surgery Research Group. Is there any benefit in using awake anesthesia with thoracic epidural in thoracoscopic talc pleurodesis? J Thorac Cardiovasc Surg. 2013;146:495-7.e1. [Crossref] [PubMed]
- Vanni G, Tacconi F, Sellitri F, et al. Impact of awake videothoracoscopic surgery on postoperative lymphocyte responses. Ann Thorac Surg. 2010;90:973-8. [Crossref] [PubMed]
- Wu CY, Chen JS, Lin YS, et al. Feasibility and safety of non intubated thoracoscopic lobectomy for geriatric lung cancer patients. Ann Thorac Surg. 2013;95:405-11. [Crossref] [PubMed]
Cite this article as: Bertolaccini L, Zaccagna G, Divisi D, Pardolesi A, Solli P, Crisci R. Awake non-intubated thoracic surgery: an attempt of systematic review and meta-analysis. Video-assist Thorac Surg 2017;2:59.


