Right sided VATS thymectomy: “current standards of extended thymectomy for myasthenia gravis”
Introduction
Endoscopic approaches for the resection of thymus in the treatment of myasthenia gravis (MG) and thymoma are increasing. In this issue of VATS journal, readers may recognize that, there is a growing experience and developing surgical technics with video-assisted thoracoscopic surgery (VATS) approaches. The classical approach is right sided VATS thymectomy which has been described many times in different journals with the accompanying videos. In right sided 3-portal VATS thymectomy, appropriate patient selection is crucial.
For appropriate patient selection, a proper radiologic examination is essential. This examination may be contrast enhanced computerized chest tomography in non myasthenic patients and magnetic resonant imaging in myasthenic patients to define the borders of resection plan.
Patient with (I) nonthymomatous MG or (II) small (<2 cm) intrathymic thymoma or (III) large but well encapsulated thymoma (preferably <5 cm) without invasion to lung, major vessels (left innominate vein being the smallest) and phrenic nerves. We prefer our patients have been examined by a qualified neurologist and anesthesiologist in MG before surgery.
Operative procedure
We prefer the right side approach for both non thymomatous MG and thymoma patients even if the thymoma is completely located on the left side. We prefer the right side because there is more room and landmarks are much clear. And also thymoma which is located on the left side maybe pulled towards the operative area after the dissection of the right thymus.
We position the patient in a 30-degree semi-supine position. The patient is supported with a roll placed under the right shoulder, and the right arm is abducted over a support attached to the table (Figure 1).
A double lumen endotracheal tube provides the lung isolation. We do not use carbon dioxide insufflation because we open the contralateral pleura for dissection of the left side. We never convert to open surgery due to hypoxemia, which is thought to be due to insufficient gas exchange of the left lung. In this situation, we immediately open the pleura and check the left upper lobe ventilation. Sometimes endotracheal tube maybe is located distal to left upper lobe so that it prevents the ventilation of the left upper lobe and causes the hypoxemia. Then the endotracheal tube is pulled back 1–2 cm after deflating the cuff of the both lumens.
Three ports are opened around the mammary gland without violating the mammalian tissue in females and from similar areas in males (Figure 2). The first port is always the camera port and a 10 mm port is inserted. A 30-degree scope is used, the left port is opened in the anterior axillary fossa lateral to the pectoralis major muscle and the right port is opened in the 5–6th intercostal space lateral to the midclavicular line. The surgeon and camera man stand side by side and the nurse stands on the other side.
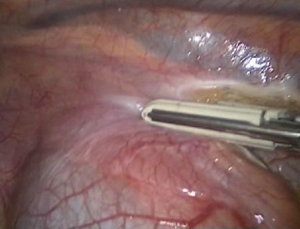
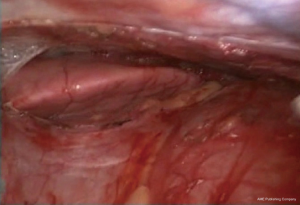
The 30° is introduced and the hemithorax is evaluated. The right phrenic nerve is defined with its relations to thymus or a thymoma. We begin the dissection with resection of the right sided pericardiophrenic fatty tissue. Then the dissection of the thymus begins by removing it from the pericardium anterior to the phrenic nerve with blunt dissection or with LigaSure™ 5 mm tissue sealer (Medtronic, Inc., Doral, FL) (Figures 3,4).
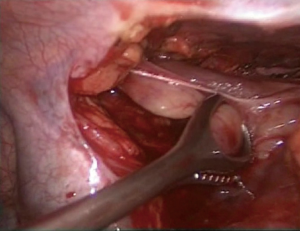
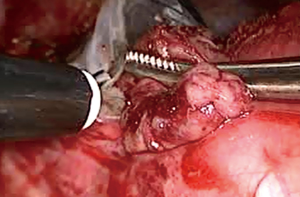
Then the thymus is dissected of the sternum by opening the mediastinal pleura along the right internal mammary artery/vein under the sternum (Figure 5). The dissection from the right side parallel to the phrenic nerve enables visualization of the superior vena cava and junction of both innominate veins clearly becomes visible. The most dangerous and accident inviting part of this operation is the dissection of the upper poles. By gentle traction on both superior poles of the thymus could be dissected and under direct visualisation (Figure 6). The superior poles dissection is best provided with gentle force applied caudally, with the use of countertraction dissection towards thyroid gland. The arterial and venous branches from the internal mammary vessels could be identified and clipped. The major thymic veins may be at different numbers and locations could be dissected and divided by clipping (Figures 7,8).

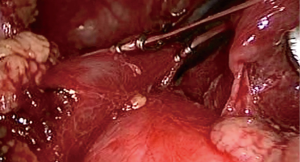
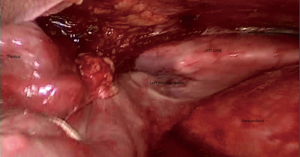
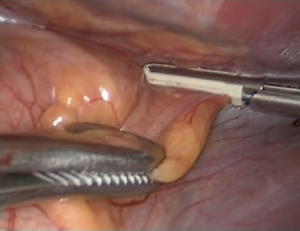
By retracting the thymus toward the right side and the dissection of the thymus is completed anteriorly and posteriorly on the right and upper half of the gland. Now, the left side of the thymus is to be dissected of the pericardium without injuring the left phrenic nerve (Figure 9). To observe the left phrenic nerve, all thymic tissue is pulled toward the surgeon and camera moved anteriorly into the left hemithoracic cavity and the dissection by the phrenic nerve is carried out (Figures 10,11). By completion of the left thymus dissection some of the fatty tissue from left pericardiophrenic angle is dissected.
The specimen is removed with an Endo bag (Figure 12). The mediastinum is carefully inspected or any foreign body or any remaining fatty mediastinal tissue or hemostasis. One 10 mm drain is placed through the most anterior port across the mediastinum to drain the both chest (Figure 13).
If the operation is carried out for a thymoma, the tumour should be dissected at the last part of the operation and surgery should be achieved with no touch technique. The non-tumorous part of the thymus is dissected first and these tissues are used for grasping and traction. Dissecting the thymoma at the last part of the operation also provides minimization of the tumor handling. Like us, many authors recommend to leave the tumor to the last part of the operation because, if the tumor is dissected first, it may cause insufficient visualization of area and contamination of the surgical field.
Discussion
Median sternotomy has been the gold standard for thymectomy (4). In the past 20 years, minimal invasive approaches are in increase in number and various technics are available (5-8).
A radical thymectomy operation can be performed with minimally invasively and patients could be discharged within the next 1 to 2 days (9). In addition cosmesis is much better compared to a sternotomy operation (10,11). To be experienced with VATS thymectomy, a surgeon should be doing non-thymomatous thymectomy at least 5–10 cases per years and completed 70 cases (12). After gaining some experience small thymomas, and then larger tumours could be resected. In MG a complete resection of thymus is crucial because it is well known that long-term clinical outcomes are related with the amount of tissue dissected.
During the surgery, identification of both phrenic nerves should be routine. Possible thermal injury to the phrenic nerves can be minimized by using a safe energy source. The superior horns are usually dissected from the innominate vein first, followed by dissection of the right horn and followed by the left horn.
Though most surgeons use three ports, routine retraction through the additional 4th medial most 5 mm port has been presented to be helpful. But, we never needed to increase the number of ports for a better exposure. The supine position is useful for quick conversion to a sternotomy but we prefer a small anterior thoracotomy, if necessary.
Acknowledgments
Funding: None.
Footnote
Provenance and peer review: The article was commissioned by the editorial office, Video-Assisted Thoracic Surgery for the series "Minimally invasive VATS thymectomy for Myasthenia Gravis". The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2017.05.02). The series “Minimally invasive VATS thymectomy for Myasthenia Gravis” was commissioned by the editorial office without any funding or sponsorship. AT served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Video-Assisted Thoracic Surgery from Aug 2016 to May 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kaba E, Cosgun T, Ayalp K, et al. Dissection of the thymus from the pericardium. Asvide 2017;4:216. Available online: http://www.asvide.com/articles/1526
- Kaba E, Cosgun T, Ayalp K, et al. The major thymic vein dissected and divided by clipping. Asvide 2017;4:217. Available online: http://www.asvide.com/articles/1527
- Kaba E, Cosgun T, Ayalp K, et al. To observe the left phrenic nerve. Asvide 2017;4:218. Available online: http://www.asvide.com/articles/1528
- Daniel VC, Wright CD. Extended transsternal thymectomy. Thorac Surg Clin 2010;20:245-52. [Crossref] [PubMed]
- Savcenko M, Wendt GK, Prince SL, et al. Video-assisted thymectomy for myasthenia gravis: an update of a single institution experience. Eur J Cardiothorac Surg 2002;22:978-83. [Crossref] [PubMed]
- Hazelrigg SR. Thoracoscopic or video-assisted (VATS) thymectomy. Op Tech Thorac Cardiovasc Surg 2004;9:184-92. [Crossref]
- Shrager JB. Extended transcervical thymectomy: the ultimate minimally invasive approach. Ann Thorac Surg 2010;89:S2128-34. [Crossref] [PubMed]
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [Crossref] [PubMed]
- Lee CY, Kim DJ, Lee JG, et al. Bilateral video-assisted thoracoscopic thymectomy has a surgical extent similar to that of transsternal extended thymectomy with more favorable early surgical outcomes for myasthenia gravis patients. Surg Endosc 2011;25:849-54. [Crossref] [PubMed]
- Mack MJ, Landreneau RJ, Yim AP, et al. Results of video-assisted thymectomy in patients with myasthenia gravis. J Thorac Cardiovasc Surg 1996;112:1352-9; discussion 1359-60. [Crossref] [PubMed]
- Lin MW, Chang YL, Huang PM, et al. Thymectomy for non-thymomatous myasthenia gravis: a comparison of surgical methods and analysis of prognostic factors. Eur J Cardiothorac Surg 2010;37:7-12. [Crossref] [PubMed]
- Toker A, Erus S, Ozkan B, et al. Does a relationship exist between the number of thoracoscopic thymectomies performed and the learning curve for thoracoscopic resection of thymoma in patients with myasthenia gravis? Interact Cardiovasc Thorac Surg 2011;12:152-5. [Crossref] [PubMed]
Cite this article as: Kaba E, Cosgun T, Ayalp K, Alomari MR, Toker A. Right sided VATS thymectomy: “current standards of extended thymectomy for myasthenia gravis”. Video-assist Thorac Surg 2017;2:30.