
Thoracoscopic pleural abrasion vs. apical pleurectomy in treatment of spontaneous pneumothorax
Introduction
Since Jakobeus performed the first thoracoscopy in 1910, the technique has developed and is currently used in the diagnostics and treatment of many diseases of the chest. It is also indisputably used in the treatment of spontaneous pneumothorax (1). However, controversies are aroused by the use of additional treatments, such as pleurodesis, abrasion or pleurectomy, while performing thoracoscopy (2).
The aim of this study is to compare the efficacy and safety of partial pleurectomy and mechanical pleural abrasion in the treatment of spontaneous pneumothorax.
Methods
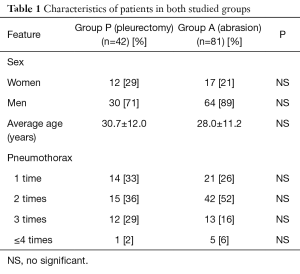
The analysis included 123 patients with spontaneous pleural pneumothorax treated with the videothoracoscopic technique (VT) in 2006–2015. There were 29 women and 94 men. The age ranged from 16 to 50 years (average: 29.3 years). In 35 cases (28%) the indication for operation was initial spontaneous pneumothorax not treated by drainage. In other cases, the indication for surgery was recurrent pneumothorax (the second episode in 57 cases, the third episode in 25 cases, and at least the fourth in 6 cases). Patients were operated on under general anaesthesia with a double lumen endotracheal tube. The triple port access was preferred. During the VT procedure the changed tissue, located mostly at the top of the lungs, was removed with a stapler and a partial pleurectomy (group P: 42 patients) or mechanical pleural abrasion (group A: 81 patients) were performed. Approval from Ethics Committee was not required for this study. Both methods—pleurectomy and pleural abrasion, are recommended in pneumothorax treatment. The selection of procedure depended on operator’s preference. Characteristics of patients in both groups are presented in Table 1. Both groups were compared in terms of the sex, size of post-operative drainage and duration of drainage, as well as post-operative complications. The obtained results were subjected to the statistical analysis using the chi square test and the Mann-Whitney U test.
Full table
Results
Both studied groups were similar in respect of the age (group P vs. A: 30.7 vs. 28, P=0.34) and sex (women P vs. A: 28% vs. 21%, P=0.16). In patients with initial emphysema, the procedure of pleurectomy was performed in 14 patients (33%) and abrasion in 21 patients (26%), P=0.95.
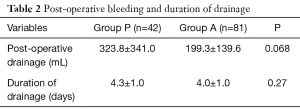
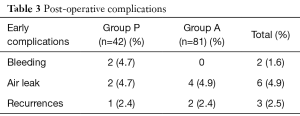
Patients in whom pleurectomy was performed had a greater post-operative drainage of blood than patients after pleural abrasion (on average 323.8 vs. 199.3 mL, P=0.068). Two patients after pleurectomy required a transfusion of 2 RbCC. In no case a conversion or repair was necessary. The average time of drainage in both groups was similar (group P vs. A: 4.3 vs. 4.0 days, P=0.27) (Table 2). Early complications occurred in 8 patients (6%). In 2 cases, there was bleeding (group P), which was treated conservatively. In 6 cases [2 (4.8%) in group P and 4 (4.9%) in group A], there was a persistent air leak, which stopped within 6–10 days. There were 3 recurrences (2.4%), 1 in group P and 2 in group A (time of observation from 1 to 10 years) (Table 3).
Full table
Full table
Discussion
Spontaneous pneumothorax occurs with an incidence of 24.0 cases in men and 9.8 cases in women per 100,000 of the population. In patients with initial emphysema at an early age there are usually small bubbles observed at the top of the lungs. Older patients and those with recurrent pneumothorax usually present the chronic obstructive pulmonary disease (2,3). The standard procedure in initial pneumothorax is a pleural drainage and the use of chemical pleurodesis. An absolute indication for VT is the recurrence of pneumothorax. There are also reports about the use of VT in the first episode of pneumothorax. Authors of those studies argue that such a conduct is associated with a low later risk of relapse (4-7). In our centre, the indication for VT is mostly recurrent pneumothorax. Exceptions are cases of initial pneumothorax in which an air leak remains for more than 5 days despite the use of pleurodesis. In our material, there were 35 patients like that (28%). VT shows an indisputable advantage over open junctures taking into account the cosmetic effect, lesser pain, shorter time of treatment and faster return to professional activity (2).
The subject of discussion is the use of additional procedures during VT: pleural abrasion, pleurectomy, pleurodesis or coagulation of bullae.
The test conducted in 2006 by Change et al. on 65 patients treated due to spontaneous pneumothorax with the VT technique showed a similar rate of complications, the need for analgesics and hospitalization time using pleural abrasion and partial pleurectomy of the mesothelioma (6). A similar result was obtained in our material. The study by Chang et al. showed 8.6% of recurrences after pleural abrasion, while in our material that percentage was 2.5%.
A 2012 randomized study on a group of 369 patients showed a greater amount of intra-operative blood loss (P=0.025) and greater post-operative drainage (P=0.04) in patients in whom pleurectomy was performed. Patients after pleural abrasion and pleurodesis complained of greater pain and required more painkillers. Both groups did not differ, however, in terms of hospitalization time and frequency of post-operative complications. The recurrence rate was the same at 3.8% (7). In our study we showed a similarly greater post-operative drainage of blood in patients in whom partial pleurectomy was performed (P=0.068). Patients after pleurectomy and pleural abrasion had a comparable duration of drainage and frequency of post-operative complications.
The study conducted by Huh and colleagues on a group of 207 patients in 2012 showed a greater rate of recurrence in patients in whom pleural abrasion was performed. Air leak occurred with similar frequency in groups of patients after pleural abrasion and pleurectomy. A similar result was obtained in our material, the patient rate with an air leak was similar at approx. 5%.
The topic of discussion is also the use of coagulation of bullae with VT treatments. The coagulation of bullae allows to reduce the number of staplers used during the procedure and reduces the costs of the treatment (8); however, according to our observations, may be the cause of a prolonged air leak.
The most common complication is a prolonged air leak, which can take place in as many as 20% of patients (9). In our material the complication was observed in 5% of patients. Pleurectomy performed during the VATS treatment can be the cause of bleeding, whose percentage may reach even 3.6%, while in other VATS procedures that percentage is at 1.9% (9,10). That complication was observed in 2 patients (1.6%). After pleurectomy we can also observe chronic post-operative pain, whose frequency reaches even 21% (10,11). Among the complications connected with pleurectomy, damage to the brachial plexus and the Horner syndrome are also described (12). That complication was not observed among our patients. Recurrences after the treatment of spontaneous pneumothorax with the VATS technique are assessed at 0 to 5% (6,9,10). In our material that percentage was 2.4% in total.
Conclusions
- The pleurectomy procedure is characterised by a greater blood loss than the pleural abrasion procedure.
- Both techniques show the same efficacy and low rate of complications in the treatment of spontaneous pneumothorax.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2017.05.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Approval from Ethics Committee was not required for this study. Individual consent for this study was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Łochowski MP, Kozak J. Video-assisted thoracic surgery complications. Wideochir Inne Tech Maloinwazyjne 2014;9:495-500. [Crossref] [PubMed]
- Huh U, Kim YD, Cho JS, et al. The Effect of Thoracoscopic Pleurodesis in Primary Spontaneous Pneumothorax: Apical Parietal Pleurectomy versus Pleural Abrasion. Korean J Thorac Cardiovasc Surg 2012;45:316-9. [Crossref] [PubMed]
- Shaikhrezai K, Thompson AI, Parkin C, et al. Video-assisted thoracoscopic surgery management of spontaneous pneumothorax--long-term results. Eur J Cardiothorac Surg 2011;40:120-3. [Crossref] [PubMed]
- Sepehripour AH, Nasir A, Shah R. Does mechanical pleurodesis result in better outcomes than chemical pleurodesis for recurrent primary spontaneous pneumothorax? Interact Cardiovasc Thorac Surg 2012;14:307-11. [Crossref] [PubMed]
- Chambers A, Scarci M. In patients with first-episode primary spontaneous pneumothorax is video-assisted thoracoscopic surgery superior to tube thoracostomy alone in terms of time to resolution of pneumothorax and incidence of recurrence? Interact Cardiovasc Thorac Surg 2009;9:1003-8. [Crossref] [PubMed]
- Chang YC, Chen CW, Huang SH, et al. Modified needlescopic video-assisted thoracic surgery for primary spontaneous pneumothorax: the long-term effects of apical pleurectomy versus pleural abrasion. Surg Endosc 2006;20:757-62. [Crossref] [PubMed]
- Chen JS, Hsu HH, Huang PM, et al. Thoracoscopic pleurodesis for primary spontaneous pneumothorax with high recurrence risk: a prospective randomized trial. Ann Surg 2012;255:440-5. [Crossref] [PubMed]
- Orki A, Demirhan R, Ciftci H, et al. Videothoracoscopic approach to recurrence primary spontaneous pneumothorax: using of electrocoagulation in small bulla/blebs. Indian J Surg 2009;71:19-22. [Crossref] [PubMed]
- Imperatori A, Rotolo N, Gatti M, et al. Peri-operative complications of video-assisted thoracoscopic surgery (VATS). Int J Surg 2008;6:S78-81. [Crossref] [PubMed]
- Gómez-Caro A, Moradiellos FJ, Larrú E, et al. Effectiveness and complications of video-assisted surgery for primary spontaneous pneumothorax. Arch Bronconeumol 2006;42:57-61. [Crossref] [PubMed]
- Passlick B, Born C, Sienel W, et al. Incidence of chronic pain after minimal-invasive surgery for spontaneous pneumothorax. Eur J Cardiothorac Surg 2001;19:355-8; discussion 358-9. [Crossref] [PubMed]
- Skoro I, Djuric K, Stancic MF. Brachial plexus injuries complicating video-assisted thoracic surgery. World Neurosurg 2011;76:208-10. [Crossref] [PubMed]
Cite this article as: Łochowski M, Brzeziński D, Pryt Ł, Rębowski M, Kozak J. Thoracoscopic pleural abrasion vs. apical pleurectomy in treatment of spontaneous pneumothorax. Video-assist Thorac Surg 2017;2:29.


