Recommendations for camera-holding during single-port video-assisted thoracoscopic lobectomy for non-small cell lung cancer
Introduction
Currently, the therapeutic effect of traditional multi-incision video-assisted thoracoscopic (VAT) surgery, which is used in the treatment of chest diseases, has been validated and accepted (1), and treatment strategies using VAT surgery has become an indispensable skill for thoracic surgeons. Even though the clinical performance of traditional multi-incision VAT surgery is similar to single-port VAT surgery (2), the latter has the advantage of reducing incisional pain and abnormal feelings post-operatively (3). As a result, this technique has been gradually applied at domestic and international hospitals (4), and will become one of the major trends in minimally invasive thoracic surgery in the future. However, this advanced technique often puzzles scholars due to the complexity of single-port thoracoscopic procedures. Mastering this specific technique not only requires excellent surgical skill, but also depends on perfect cooperation with an experienced mirror assistant. The current study summarizes the current understanding of single-port thoracoscopic lobectomy and mediastinal lymph node dissection. Based on the author’s experience as an assistant holding the camera at Fujian Medical University Union Hospital between May 2014 and June 2016, the specific coordination skills of single-port thoracoscopy, the difficulties of a mirror assistant, and possible solutions to problems are described.
Methods
Patients
Between May 2014 and June 2016, the author took part in 82 single-port VAT lobectomies as the camera holder. Mediastinal lymph node dissections were performed in all cases. The study was approved by ethics committee of Fujian Medical University Union Hospital (No.2016KY037) and written informed consent was obtained from all patients. The patients’ characteristics are presented in Table 1.

Full table
Anesthesia
Combination intravenous-inhalation anesthesia was administered to all patients. The ventilation strategy was double-lumen tube intubation with normal side pulmonary ventilation.
Incision design
A 3–4 cm incision was typically made in the 4th intercostal space at the mid-axillary line of the affected side. For slender patients, the incision was sometime made in the 5th intercostal space.
Operative process
The specific operative process of single-port VAT lobectomy has been summarized in our previous report (5). A standard mediastinal lymph node dissection was performed. Stations 2, 3, 4R, 7, 8, and 9 were dissected for right pulmonary procedures and stations 4L, 5, 6, 7, 8, and 9 were dissected for left pulmonary procedures.
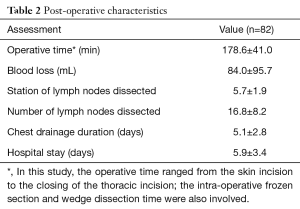
Results
Post-operative data, including operative time, blood loss, number of lymph nodes dissected, chest drainage duration, and hospital stay, are presented in Table 2.
Full table
Discussion
Single-port thoracoscopic lobectomy and mediastinal lymph node dissection strategies
The rotating thoracoscope is the “eyes” of the laparoscopic surgical team, and thoracoscopic surgery is a team effort, requiring not only the skilled operating practices of a surgeon, but also good strategies of the mirror assistant. The surgery can be affected by the quality of the rotary mirror from various aspects, including the comfort and mood of the primary surgeon, the fluency of surgery, the ornamental value of the surgery, and most importantly, the safety of the procedure. For single-port VAT surgery in particular, the strategy of the mirror assistant is important due to the potential interference between the lens and other instruments.
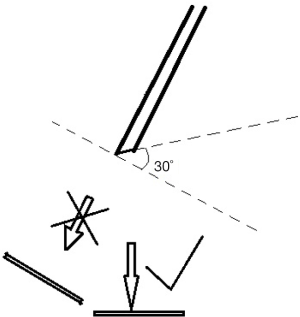
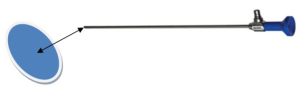
Structure and imaging principles of the thoracoscope
The basic structure of the thoracoscope and the imaging principles should be introduced before use. The thoracoscopic imaging lens system can be used by placing the thoracoscopic lens into the thoracic cavity. The images that are taken will transmit to the post-stage signal processing system by the optical fiber and be displayed on a dedicated monitor in real time. The physicians subsequently evaluate the patient’s condition, make judgements through images of the patient’s organs in different angles on the monitor screen, and prepare the chest before surgery. Currently, a thoracoscope with a 30-degree angle has been widely used in clinical practice. The obtained image is located anterior-inferior of the lens rather than in front of the lens (Figure 1).
Preparation of the thoracoscope before surgery
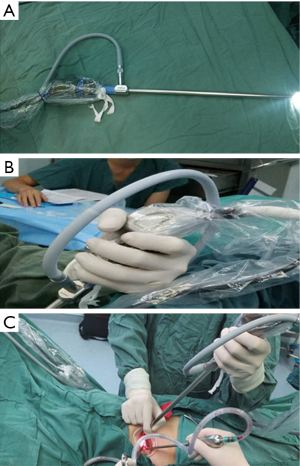
Fixing guide light beams
The guide light beam is fixed along the back side of the patient and tied with a thread to the tail of the camera to prevent guide light beams from rotation by gravity and reduce the interference between the thoracoscope and the surgical procedure (Figure 2).
Thoracoscope anti-fogging treatment
Boiling water is used to immerse the lens for at least 5 seconds. If conditions permit, the hot water should be changed, minimize the time of lens fogging, and ensure a seamless operative procedure. The lens wiping order is as follows: mirror; body; soak in hot water; mirror; and body.
The position of the camera holder
The position of the camera holder may be ipsilateral or contralateral based on the team habit. Our experience has shown that the opposite position may be better (Figure 3). Thus, the surgeon stands on the ventral aspect and the camera holder stands on the dorsal aspect. The advantage of the contralateral station is less body interference between the primary surgeon and the camera holder, which permits more space for the procedure. In contrast, the major drawback of the contralateral station is the opposite direction between images posterior to the mediastinum and the lower half of the chest requires additional time for adaptation.

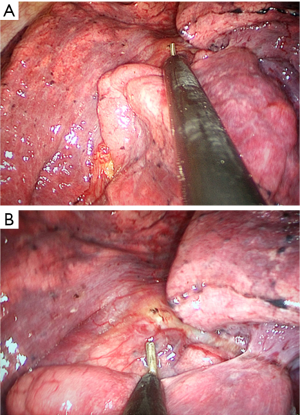
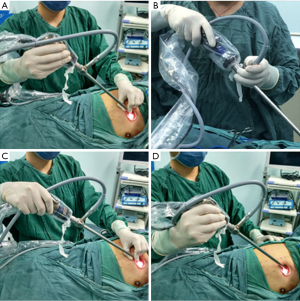
Approaches of rotating the thoracoscope
There are two approaches for rotating the single-port thoracoscope, including the single- and two-hand thoracoscope methods. The former method is considered the norm and suitable for a long procedure by avoiding fatigue (Figure 4A,B), whereas the latter method is suitable for a short procedure as it is readily causes fatigue, especially when assistance is required for exposure during the operation (Figure 4C,D).
Basic principles of rotating the thoracoscope
Vertical images with respect to the primary surgeon direct the rotation of the thoracoscope. The endoscope body is close to the incision (Figure 5) above (the patient’s dorsal part) to give incision space for the surgeon in an attempt to maintain a stable image, adjusting the viewing distance of the camera and focal length to obtain a clear image.
Senior strategies of the rotating thoracoscope
Control of image stability
For the same surgical field, a clear image can be acquired using a fixed focal length and maintaining a specific distance between the target and the lens (Figure 6). The image appears blurred while maintaining the lens caused by an unfixed focal length when the distance between the lens and the observed object is changed. Consequently, the distance between the lens and the observed object should be restored to original condition or adjust the focus.
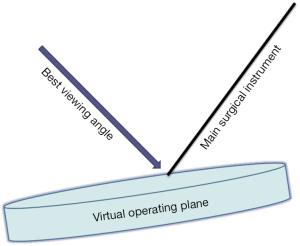
Principle of the best viewing angle
Each of the surgical fields can be a virtual operating plane, and the angled diagonal between the main surgical instruments, such as the electricity hook, ultrasonic knives, and operating plane, is the best viewing angle (Figure 7), which requires a closer view of the distance in the single-port VAT surgery for obtaining the best viewing angle. The process of rotating the thoracoscope should be adjusted in accordance with this principle, which achieves the best stereo vision, thus making the head of the energy operating instrument and the structures of the surrounding tissues present the clearest positional relationship to avoid the “with feelings” operation and improve surgical safety.
The principle of instruments cross
The operative instrument attempts to be crossed as much as possible when it is inserted into the incision, thus minimizing the interference between the thoracoscope body and the operating instruments (Figure 8).
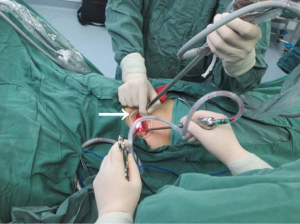
Coordination of the surgical exposure
The single-port VAT surgery often needs an assistant to manipulate instruments for exposure during surgery. The rotating thoracoscope and other instruments are held by an assistant to maximize surgical exposure. In addition, the assistant needs to place the instrument to provide exposure at the incision, fix the lens above the incision, and effectively alleviate fatigue by rotating the thoracoscope (Figure 9).
Fluency of surgery
In order to make surgery more fluent, the rotating thoracoscope assistant should also pay attention to relieving fatigue, be familiar with the detailed steps and habits of the primary surgeon, and at the same time, coordinate with the team long-term. Excellent cooperation in the team will make the operation smooth, fast, and safe.
Difficulties in the surgery and its solutions
Tips for cleaning the mirror
Wiping the lens and lens body (excluding blood) with a dry cloth before washing the lens, then soaking the lens and lens body in hot water, and wiping the lens and lens body.
“Arrow” effect and inability to determine the specific anatomic level
Without affecting the operation, closer observation can effectively eliminate the “arrow” effect (Figure 10).
Blurred images have many causes
The lens should be cleaned when the camera is polluted by tissue fluid, possibly caused by the proximity between the lens and tissues; pulling the lens away from tissues helps to reduce the frequency of lens pollution. A foggy mirror can be cleared by using the aspirator and soaking the lens in hot water. The change in the distance between the lens and observation target can be managed by adjusting the focal length or restoring the original distance (the distance between the lens and the observation target).
The selection and the location of instruments
Obvious interference between the thoracoscope and instruments renders surgical procedures difficult. According to the principle “one is bent, the other is straight and one is long, the other is short”, the selection of instruments should be a straight, bent, long, and short instrument. The selection of surgical instruments can effectively reduce the frequency of interference. The farthest distance between the lens body and operating instruments minimum interference principle, and the optimum angle of rotating the thoracoscope should take into account the distance between the thoracoscope and the operating instruments. The farther the distance, the less the interference, and the smoother the operation (Figure 11).
If the surgical field cannot be placed in the center of the image, the viewing distance should be adjusted, the optical fiber should be rotated, and the viewing direction changed. The method is most commonly used and practical; however, when none of these solutions solve the problem, re-arrangement of each instrument position should be considered.
The taboos of rotating the thoracoscope
Avoiding stirring when dissecting, and freeing and breaking blood vessels and other important structures. If the structure cannot be seen clearly, a safe practice is to move forward or backward along the vertical axis of the thoracoscope to avoid damaging blood vessels and other important tissues. The thoracoscope should be moved around to avoid collision with operating instruments, and the assistant is prohibited from removing the lens when an emergency occurs, such as bleeding, to prevent uncontrolled bleeding.
In conclusion, in addition to the surgeon’s skillful manipulation, tacit cooperation between the camera holder and surgeon is important for the successful completion of single-port VAT lobectomies. A clear mind and rapid reaction to intra-operative technical challenges by the camera holder will help ease the difficulty of single-port VAT surgery.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2017.03.09). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of Fujian Medical University Union Hospital (No.2016KY037) and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li Y, Sui XZ, Jiang ZC, et al. Experience of completely video-assisted thoracoscopic lobectomy in non-small cell lung cancer: series of consecutive 500 patients in single-center. Chin J Thorac Cardiovasc Surg 2012;28:3-6.
- Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg 2016;5:76-84. [Crossref] [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [Crossref] [PubMed]
- Chen D, Du M, Yang T. Uniportal video-assisted thoracoscopic lobectomy for lung cancer. J Thorac Dis 2016;8:1830-3. [Crossref] [PubMed]
- Zhu Y, Xu G, Zheng B, et al. Single-port video-assisted thoracoscopic surgery lung resection: experiences in Fujian Medical University Union Hospital. J Thorac Dis 2015;7:1241-51. [PubMed]
Cite this article as: Xu G, Chen H, Zheng B, Zheng W, Zhu Y, Guo Z, Chen C. Recommendations for camera-holding during single-port video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Video-assist Thorac Surg 2017;2:24.