
Biportal VATS approach in the treatment of penetrating thoracic trauma: a case report
Introduction
Penetrating chest trauma is less common but more deadly than blunt chest trauma. Thoracic wall penetration from stabbings comprises up to 9.5 percent of all major trauma in the United States (1) with a high mortality rate of about 30% (2). Thoracotomy has been considered the standard method for treating penetrating chest injuries owing to its safety and proper exposure of the intrathoracic cavity; on the other hand, the full role of VATS in the management of stab injuries of the chest is still a subject of debate. We report the case of a patient with penetrating chest trauma and laceration of the pulmonary middle lobe successfully treated by a biportal VATS approach.
Case presentation
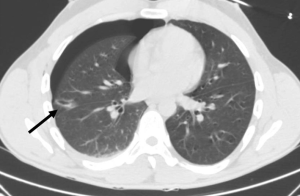
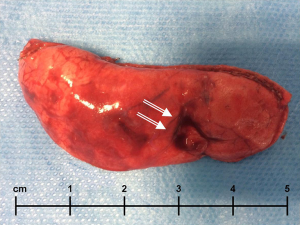
The Emergency Department referred a 30-year old Caucasic man with a stab wound to the right chest to our Thoracic Surgery Unit. Medical history was positive for asthma and active smoking. Physical examination showed a single stab wound to the right chest, 1 cm in diameter, at the fifth intercostal space (at the level of the anterior axillary line), without significant subcutaneous emphysema. Lung auscultation revealed decreased breath sounds in the whole right hemithorax. Haemodynamic parameters were normal: arterial blood pressure of 140 (systolic)/90 (diastolic) was detected without tachycardia nor tachypnea. Arterial blood gases (ABG) showed a partial oxygen pressure (PO2) of 82 mmHg, a PCO2 of 37 mmHg, and pH of 7.41; arterial oxygen saturation (SaO2) was 95%. A blood test revealed a haemoglobin of 11.5 g/dL. A Chest CT-Scan with contrast medium was performed, showing a 5-cm right pneumothorax with ipsilateral haemothorax and a penetrating laceration of the middle lobe (Figure 1), with a light active bleeding. The patient was taken to the operating room; we planned to start a VATS procedure with the patient in the left hemilateral decubitus position and double-lumen endobronchial tube ventilation. A first pleurotomy through the right 7th intercostal space on the anterior axillary line, using a 5-mm trocar was performed. A rigid 30° video-thoracoscope was passed; we observed a single penetrating and bleeding laceration of the middle pulmonary lobe and about 600 mL of blood that was removed from the right chest cavity. No other injuries were detected at a more careful thoracoscopic exploration. A right mini-thoracotomy (3 cm) was then performed at the level of the chest stab wound (at the 5th intercostal space) to allow the endoscopic equipment and the staplers to move inside; ribs divarication was avoided. A wedge lung resection of the lateral segment of the middle lobe, including the damaged and bleeding lung portion, was carried out (Figure 2). A single chest tube was placed at the level of the lower thoracoscopy port. The post-operative period was uneventful. The chest tube was removed on Post-Operative-Day (POD) 4; the Chest-X-rays after chest tube removal showed optimal lung re-expansion. The patient was discharged on POD five.
Discussion
Chest trauma patients are managed with tube thoracostomy (3); thoracotomy is infrequent required, and pulmonary resection is a rare eventuality. However, in a series reported by Stewart et al. (4), 14 of 32 patients with a stab wound underwent a pulmonary resection by a thoracotomy approach. Many thoracic surgeons believe that thoracotomy is the standard method for treating penetrating chest trauma with visceral injuries also in haemodynamically stable patients (5). During the last few years, VATS has become an increasingly popular approach to managing most thoracic diseases, and VATS is performing nowadays complex pulmonary resections. The experience acquired in the last ten years in VATS surgery, as well as the development and improvement of thoracoscopic equipment (especially endoscopic staplers and high definition cameras), has contributed to change the opinion of the latest generation of surgeons (6). The importance for VATS in the treatment of chest trauma is enhanced by other Authors regarding a more favourable postoperative course and outcome (7); on the other hand, the role of VATS in repairing lung lacerations is also confirmed in blunt chest trauma (8). Pons et al. (9) report their experience of video thoracoscopy in stable hemodynamic patients at risk of suffering a penetrating cardiac injury; in this context VATS is proposed as a good alternative to the subxiphoid pericardial window, to make a diagnosis of heart injury and perform other procedures like hemostasis of parietal vessels, reparations of diaphragm, removal of foreign bodies. These results confirm a central role of VATS in the management of penetrating chest injuries. The central point is the selection of patients suitable for a mini-invasive surgical approach. According to Ben-Nun et al. (7), there are three major criteria to be met before approaching a chest trauma with VATS: (I) hemodynamically stable patients; (II) complete pre-operative imaging in the absence of specific findings necessitating open surgery; (III) complete clinic records documentation with a medical history without absolute contraindications to VATS. Following the experience gained in minimally invasive treatment of lung cancer, we believe it is important to minimise surgical aggressiveness also in patients with penetrating chest trauma and visceral injury, with a hemodynamically stable condition and without any great vessel or cardiac lesions suspected or confirmed by the chest CT-Scan.
Conclusions
In hemodynamically stable patients with complete pre-operative imaging, in the absence of specific indications to thoracotomy, and without absolute VATS contraindications, a minimally invasive approach by a skilled surgeon could be performed safely with low postoperative morbidity, lower incidence of the wound and pulmonary complications, a shorter hospitalisation and greater patient satisfaction.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2017.02.04). LB serves as an unpaid editorial board member of Video-Assisted Thoracic Surgery from Jul 2016 to May 2019. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient. A copy of the written consent is available for review by the Editors-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Champion HR, Copes WS, Sacco WJ, et al. The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma 1990;30:1356-65. [Crossref] [PubMed]
- Clarke DL, Quazi MA, Reddy K, et al. Emergency operation for penetrating thoracic trauma in a metropolitan surgical service in South Africa. J Thorac Cardiovasc Surg 2011;142:563-8. [Crossref] [PubMed]
- Pickard LR, Mattox KL. Thoracic trauma and indications for thoracotomy. In: Mattox KL, Moore EE, Feliciano DV, editors. Trauma. Norwalk: Appleton and Lange; 1980:315-20.
- Stewart KC, Urschel JD, Nakai SS, et al. Pulmonary resection for lung trauma. Ann Thorac Surg 1997;63:1587-8. [Crossref] [PubMed]
- Richardson JD, Miller FB, Carrillo EH, et al. Complex thoracic injuries. Surg Clin North Am 1996;76:725-48. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Ben-Nun A, Orlovsky M, Best LA. Video-assisted thoracoscopic surgery in the treatment of chest trauma: long-term benefit. Ann Thorac Surg 2007;83:383-7. [Crossref] [PubMed]
- Chou YP, Kuo LC, Soo KM, et al. The role of repairing lung lacerations during video-assisted thoracoscopic surgery evacuations for retained haemothorax caused by blunt chest trauma. Eur J Cardiothorac Surg 2014;46:107-11. [Crossref] [PubMed]
- Pons F, Lang-Lazdunski L, de Kerangal X, et al. The role of videothoracoscopy in management of precordial thoracic penetrating injuries. Eur J Cardiothorac Surg 2002;22:7-12. [Crossref] [PubMed]
Cite this article as: Lo Faso F, Davoli F, Bagioni P, Bertolaccini L, Solli P. Biportal VATS approach in the treatment of penetrating thoracic trauma: a case report. Video-assist Thorac Surg 2017;2:8.


