Video-assisted thoracic surgery tunnel technique: an alternative fissureless approach for anatomical lung resections
Introduction
During lung surgery, surgeons use mechanical staplers on the fissural parenchyma between different lobes to minimize the chance of postoperative prolonged airleak. Many video-assisted thoracic surgery (VATS) surgeons use a “hilum first, fissure last technique”. The hilar bronchovascular structures are divided first and during the last step of the lobectomy the lobe is lifted and the fissural parenchyma is divided. Thanks to these fissureless techniques, incomplete or fused fissures are no longer contraindications for VATS anatomical resections (1,2).
Some VATS surgeons and many robotic surgeons continue to reveal the artery by dissecting into the fissural parenchyma. This technique, similar to open surgery, allows surgeons to remove N1 nodes on the artery and bronchus first, and to look for anatomical variations before starting to divide the bronchovascular structures. But, dissecting into the incomplete fissure can cause prolonged airleak.
The objective of this paper is to present an alternative fissureless technique, combining the advantages of the techniques described above.
Methods
Technique
General principles
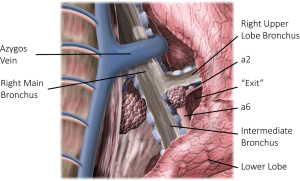
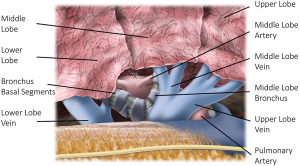
The objective of the presented technique is to open an incomplete interlobar fissure with staplers before bronchovascular structures are divided (3). This can be achieved by making a tunnel between the bronchovascular structures and the parenchyma. We will only describe the technique to make this tunnel from anterior to posterior, although the other way around is also possible. For all three fissures, the technique starts with dissection between the lobar veins, removing all fat and lymph nodes. Next, dissection is continued between the bronchi (except for the horizontal fissure) and between the artery and the parenchyma. It is important to visualise the artery. Only then, the tip of a stapler should to be placed peripheral/lateral of the artery. It is important to keep the stapler steady and to pull the parenchyma into the stapler. Firing the stapler will open the anterior part of the incomplete fissure. Further dissection continues over the artery. The ideal dissection plane is close to the artery. Therefore, all connective tissue should be removed until the artery is free. In our experience, freeing the “exit” of the tunnel first, makes the procedures much easier. On the left side this exit is located at the artery, more specific, between the artery of the posterior segment (a2) and the apex of the lower lobe (a6) (Figure 1). On the right, the exit can be found at the secondary carina between upper lobe bronchus and intermediate bronchus (Figure 2).
Our routine VATS technique is a common three port technique, similar to Hansen et al. (4). We often tilt the table anterior to better expose the posterior side of the hilum. The described technique can be performed multiportal, uniportal or robotic. But, camera view of the posterior side of the hilum is very helpful and the anterior to posterior view in the direction of the oblique fissure is essential.
Once the fissure is completed, a complete view on the bronchovascular anatomy is obtained. The anatomical resection, lobar or segmental, can then be performed in a smooth and safe manner.
Left oblique fissure (Table 1)
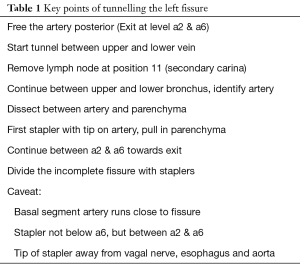
Full table
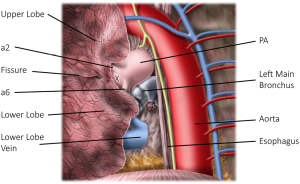
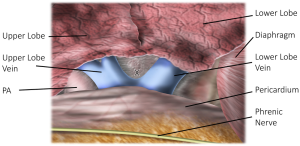
Transection of the lower pulmonary ligament exposes the lower pulmonary vein. Further opening of the posterior pleural reflexion reveals the pericardium, left main bronchus and pulmonary artery (PA) (Figure 1). We typically tilt the table anteriorly to achieve perfect exposure to the posterior hilum. Removing the connective tissue and lymph nodes over the artery and bronchus will bring the lung out of the mediastinum and gives easier access to the subcarinal nodes. We free the artery until we notice the origin of both the artery towards the posterior segment of the upper lobe (a2) and the apex of the lower lobe (a6). The exit of the tunnel lies between both.
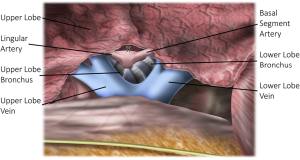
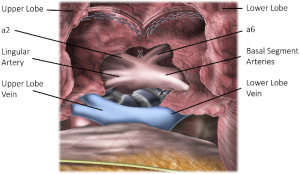
Then we change the camera view to a common anterior to posterior direction in line with the oblique fissure (Figure 3). We identify the upper and lower vein, open the pleural reflexion and remove hilar fat and nodes. This usually exposes the lower lobe bronchus. More cranially the secondary carina between the lower and upper lobe bronchus can be found. If necessary, the upper lobe vein should be retracted. Removal of the nodes at position 11 at the secondary carina reveals the PA (Figure 4). Pushing up the parenchyma over the artery creates the plane for the tunnel. The anvil of a 60 mm stapler is placed with the tip between the artery and parenchyma. The parenchyma is pulled into the stapler, while the tip is held in place. The anterior portion of the oblique fissure is divided. Then, dissection between artery and parenchyma is continued. The lingular and basal arteries are identified and dissection over the main PA will end at the posterior and apical branches (a2 and a6) (Figure 5). The previous posterior dissection over the artery will greatly help to complete the tunnel. Overlying lymph nodes should be removed. With the next staplers the middle and posterior part of the fissure is opened.
After division of the fissure, the rest of the lobectomy can be performed swiftly and safely as the structures are mostly freed. For a left upper lobe, our typical sequence is the division of the lingular artery, the upper lobe vein, the upper lobe bronchus and finally the remainder of the arteries. For a left lower lobe this can be vein or artery first and finally the bronchus.
Right sided fissures
The fissures on the right can be divided in the anterior oblique fissure between middle lobe and lower lobe; the posterior oblique fissure between lower lobe and upper lobe, and the horizontal fissure between middle lobe and upper lobe.
Often the fissure is well developed at the intersection of these three parts. The artery can be found superficial under connective tissue. If so, opening the posterior part of the oblique fissure can be started at this point. If not, the anterior part can be opened first with a tunnel technique.
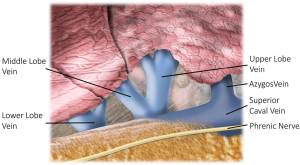
Transection of the lower pulmonary ligament exposes the right lower vein. We then tilt the table towards anterior to have a nice exposure of the posterior hilum. The pleural reflexion is opened all the way up, ending at azygos vein which is freed from the main bronchus. Removal of connective tissue brings the lung out of the mediastinum and eases the resection of the subcarinal nodes. The end of the oblique fissure can be found at the secondary carina formed by the upper lobe bronchus and the intermediate bronchus (Figure 2). Pushing the parenchyma laterally at this level reveals the exit of the tunnel under the posterior part of the incomplete oblique fissure. When the position 11 node at the secondary carina is removed, the artery towards the posterior segment of the upper lobe can be seen (a2). This will significantly help to complete the division of the posterior part of the fissure (5).
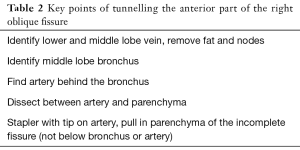
Right oblique fissure, anterior part (Table 2)
Full table
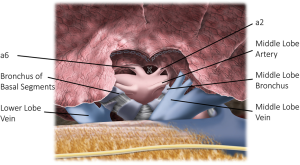
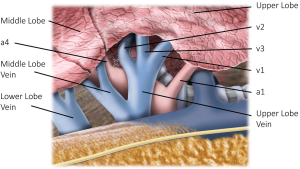
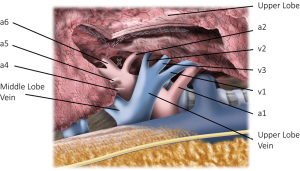
Switching to an anterior view, the veins of the lower lobe, middle lobe and upper lobe should be recognized (Figure 6). Between the lower lobe and middle lobe vein, fat and nodes needs to be removed to find the bronchus to the middle lobe. When this bronchus is followed centrally and towards posterior, the bronchus to the basal segments can be found. Between these bronchi, the PA can be revealed (Figure 7). Dissection between the artery and parenchyma is the plane to be followed to create the tunnel. The anvil of a 60 mm stapler is placed on top of the artery. The anterior part of the incomplete oblique fissure is pulled into the stapler and divided. This results in a better view on the artery.
Right oblique fissure, posterior part (Table 3)
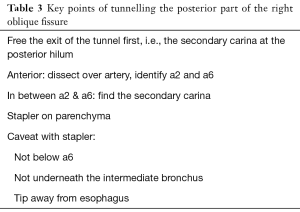
Full table
To open the posterior part of the oblique fissure, the artery in the fissure should be freed first. This can be done by opening the anterior part of the oblique fissure as described above. In case of a good quality fissure at the junction of the three fissures, the artery can sometimes be exposed without parenchymal tears. In case of a right upper lobectomy, we divide the horizontal fissure first and continue with the posterior part of the oblique fissure.
After exposing the PA, the origins of a middle lobe artery and the basal segment arteries are identified and overlying lymph nodes removed. Further dissection between the artery and parenchyma reveals the segmental branch to the apex of the lower lobe (a6) and the posterior ascending branch to upper lobe (a2). With staplers, the central part of the fissural parenchyma is divided. Next the tunnel is completed over the artery, in the direction of the previously freed secondary carina, which is the exit of the tunnel (Figure 8). If the position 11 node in the secondary carina was not removed completely, one can remove it after completion of the division of the fissure with a third stapler.
Right horizontal fissure (Table 4)
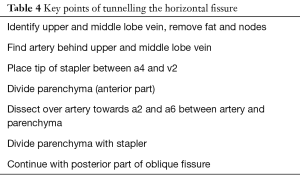
Full table
A right upper lobectomy requires the division of the horizontal fissure and the posterior part of the oblique fissure. Therefore, the first steps can be similar to a lower lobectomy with posterior release of the hilum, exposure of the bronchus and the secondary carina with removal of the lymph node there (Figure 2).
The middle lobe and upper lobe veins are identified from an anterior view (Figure 6). The veins that are draining the upper lobe are encircled, with care for the PA just posterior to it. Removal of fat and nodes and further dissection between the parenchyma and the confluence of both veins will reveal the PA behind the middle lobe vein. The further line of dissection is between the middle lobe artery (a4) and the vein draining the posterior segment of the upper lobe (v2) (Figure 9). Dissection close to the artery, between the artery and the parenchyma clears the plane of the tunnel. The tip of a 60 mm stapler is placed on top of the artery and the parenchyma of the horizontal fissure is pulled into the stapler. The division of the fissure will help visualize the inferior part of the PA, including the posterior ascending branch of the upper lobe (a2) (Figure 10). Sometimes the a2 is absent, very small or more anterior than anticipated. Dissection between parenchyma and artery ends at the previously exposed secondary carina, completing the tunnel. At that time, the posterior part of the oblique fissure is divided.
Discussion
Dividing the parenchyma overlying the artery in the fissure can result in postoperative air leak, even in patients with nearly complete fissures. In VATS lobectomy patients, with an overall faster recovery and shorter hospital stay, the occurrence of an air leak might have more impact in comparison with thoracotomy patients with an overall longer hospital stay.
The use of staplers to divide incomplete interlobar fissures significantly reduces the duration of postoperative air leak and hospital stay compared with cautery (6,7). The level of completeness of lobar fissures is highly variable. A high-resolution CT analysis of 250 patients showed an incomplete main fissure on the left side in 24%, on the right in 35% and incomplete horizontal fissure in 74% (8). This results in a higher risk of postoperative air leak after right upper lobectomy compared with other lobectomies (9).
A fissureless technique by thoracotomy was published by Temes et al. Instead of dividing the overlying parenchyma to expose the PA in the fissure, the parenchyma was divided from posteriorly to anteriorly with staplers at an early stage of the operation. They indicated that they developed the fissure completely before bronchovascular structures are divided, except for the right upper lobe (10).
Gomez-Caro described a fissureless technique where, for the upper lobes, the vein is transected first, next the first branches of the PA, the bronchus and then the posterior ascending or lingular artery. Finally, the fused fissure is stapled (11). This is known as a “hilum first, fissure last” technique.
With the rise of VATS with a superior lateral view on the hilum, it became more obvious to transect the hilar structures first and, in a final step of the lobectomy, to divide the incomplete fissure. Nomori et al., Mitchell, Hansen et al. and Balsara et al. described a VATS “hilum first, fissure last” or “fissure no touch” technique (1,4,5,12).
However, we see several advantages in learning a VATS technique that helps to open fissures with staplers in an early stage of the operation.
- Mastering the “tunnel”-technique offers an alternative option when problems with a hilum first technique arise. This can be an incomplete fissure in combination with a technical issue that obstructs the “hilum first” technique: e.g., a central tumour, a tumor involved lymph node or a (near) bleeding of the anterior trunk of the PA;
- Opening the fissure with staplers in an early stage of the operation greatly facilitates VATS segmental resections;
- A clear view of the intrafissural anatomy protects against erroneous transections of bronchovascular structures;
- The lobectomy after the “tunnel” technique can be done with minimal retraction of the lung. Once the fissure is open, the weight of the lobes keeps the fissure exposed;
- As all bronchovascular structures are identified before the anatomical resection starts, one can divide the artery quickly after the vein. It diminishes the chances of a congestion of the lobe, obscuring the view;
- Gomez-Caro stated that the “hilum first, fissure last” technique is not suitable for central tumours or patients with N1 disease (11). In contrast, when making a tunnel between artery and parenchyma, undermining and ultimately dividing the fissure, it is more evident not to miss the position 11 nodes, be it in the secondary carina or next to the artery.
We previously published a cohort of 198 consecutive patients operated with this alternative fissureless technique demonstrating the feasibility and non-inferiority regarding hospital stay, chest tube duration, operation time and complications in comparison with the hilum first technique (3). Since then, we continued to use the tunnel technique with early division of the lobar fissures with staplers as our standard VATS technique.
Conclusions
The depicted “tunnel”-technique involves early opening of the fissures with staplers during VATS anatomical resections.
For surgeons who normally use a hilum first, fissure last technique, this is an alternative option, when the hilar route is being “obstructed” by a central tumour, involved lymph node or (potential) bleeding. For surgeons who are used to dissecting into the fissure first to find the artery, we believe it is a valuable technique to open the fissure entirely with staplers, diminishing the chance of postoperative air leakage. Intrafissural N1 nodes are easily detected and removed. We think that this technique gives a superior view on the intrafissural anatomy before resection is started. This helps to detect anatomical variations, to perform segmental resections and to reduce the chance of inadvertent transections.
Acknowledgments
Many thanks to Dr. Youri Sokolow, Dr. Frederic De Ryck, Dr. Alessia Stanzi, Dr. Lieven Depypere and Prof. Dr. Paul De Leyn for their valued comments on the drawings.
Funding: This manuscript was supported by a grant from Funds for Research-Flanders to Herbert Decaluwe (FWO 1701018N).
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Dominique Gossot) for the series “Video-assisted major thoracic procedures: Approaches” published in Video-Assisted Thoracic Surgery. The article has undergone external peer review.
Conflicts of Interest: The series “Video-assisted major thoracic procedures: Approaches” was commissioned by the editorial office without any funding or sponsorship. The author received Speaker’s fee from Medtronic.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nomori H, Ohtsuka T, Horio H, et al. Thoracoscopic lobectomy for lung cancer with a largely fused fissure. Chest 2003;123:619-22. [Crossref] [PubMed]
- Hanna JM, Berry MF, D’Amico TA. Contraindications of video-assisted thoracoscopic surgical lobectomy and determinants of conversion to open. J Thorac Dis 2013;5:S182-9. [PubMed]
- Decaluwe H, Sokolow Y, Deryck F, et al. Thoracoscopic tunnel technique for anatomical lung resections: a 'fissure first, hilum last' approach with staplers in the fissureless patient. Interact Cardiovasc Thorac Surg 2015;21:2-7. [Crossref] [PubMed]
- Hansen HJ, Petersen RH, Christensen M. Video-assisted thoracoscopic surgery (VATS) lobectomy using a standardized anterior approach. Surg Endosc 2011;25:1263-9. [Crossref] [PubMed]
- Balsara KR, Balderson SS, D'Amico TA. Surgical techniques to avoid parenchymal injury during lung resection (fissureless lobectomy). Thorac Surg Clin 2010;20:365-9. [Crossref] [PubMed]
- Venuta F, Rendina EA, De Giacomo T, et al. Technique to reduce air leaks after pulmonary lobectomy. Eur J Cardiothorac Surg 1998;13:361-4. [Crossref] [PubMed]
- Tantraworasin A, Seateang S, Bunchungmongkol N. Staplers versus hand-sewing for pulmonary lobectomy: randomized controlled trial. Asian Cardiovasc Thorac Ann 2014;22:309-14. [Crossref] [PubMed]
- Proto AV, Ball JB Jr. Computed tomography of the major and minor fissures. AJR Am J Roentgenol 1983;140:439-48. [Crossref] [PubMed]
- Ng T, Ryder BA, Machan JT, et al. Decreasing the incidence of prolonged air leak after right upper lobectomy with the anterior fissureless technique. J Thorac Cardiovasc Surg 2010;139:1007-11. [Crossref] [PubMed]
- Temes RT, Willms CD, Endara SA, et al. Fissureless lobectomy. Ann Thorac Surg 1998;65:282-4. [Crossref] [PubMed]
- Gómez-Caro A, Calvo MJ, Lanzas JT, et al. The approach of fused fissures with fissureless technique decreases the incidence of persistent air leak after lobectomy. Eur J Cardiothorac Surg 2007;31:203-8. [Crossref] [PubMed]
- Mitchell JD. Techniques of VATS lobectomy. J Thorac Dis 2013;5:S177-81. [PubMed]
Cite this article as: Decaluwé H. Video-assisted thoracic surgery tunnel technique: an alternative fissureless approach for anatomical lung resections. Video-assist Thorac Surg 2017;2:45.